( Synonyms: Hunter syndrome, mucopolysaccharidosis type II, MPS II, MPS 2, iduronate-2-sulfatase deficiency, IDS deficiency, mild form known historically as gargoylism)

The mucopolysaccharidoses are a group of inherited lysosomal storage diseases.There is an accumulation of incompletely degraded glycosaminoglycans (acid mucopolysaccharides) in tissues, in this case heparan and dermatan sulfate. Glycosaminoglycans are polysaccharide chains containing amino-sugars that are part of the structure of proteoglycans. Proteoglycans play an important structural and functional role throughout the body. They consist of a central protein core with multiple glycosaminoglycan polysaccharide chains attached. Proteoglycans are found intracellularly, on the cell surface, as part of the extracellular matrix and in basement membranes. Their roles are thought to be varied and largely undefined, predominantly of structural importance. In cartilage, proteoglycans play an important role in its 'shock-absorber' function by retaining water to form a yielding sponge-like structure. They have a complex biosynthetic pathway and are degraded by specific enzymes, one for each particular type of glycosaminoglycan chain.
In Hunter's syndrome the deficient enzyme is iduronate-2-sulfatase (I2S), that catalyzes the hydrolysis of asparagine and N-acetylglucosamine in heparan sulfate and dermatan sulfate . In unaffected people, these enzymes are found in parts of the body's cells known as lysosomes. The lysosomes use enzymes to break down glycosaminoglycans, as part of the body's normal recycling and renewal process. Normally, the nutrients that are broken down by lysosomes help your body build bone, cartilage, tendons, corneas, skin and connective tissue, and the fluid that lubricates your joints.
When this enzyme isn't working properly, undigested glycosaminoglycans collect in the cells, blood and connective tissues, causing permanent and progressive damage. Not all people with Hunter syndrome are affected by the disease in exactly the same way, and the rate of symptom progression varies widely. However, Hunter syndrome is always severe, progressive, and life-limiting.

Heparan sulfate catabolism involving GlcNS3S structures. The scheme illustrates all nine different enzymatic activities required for the sequential catabolism of a NRE tetrasaccharide containing GlcNS3S. To expose the 3-O-sulfated residue at the terminus, the preceding uronic acid (iduronate 2-O-sulfate in this example) is modified sequentially by iduronate 2-sulfatase and iduronidase. Under normal conditions, the 3-O-sulfate then is removed from GlcNS3S by ARSG, thus generating the substrate for sulfamidase, which removes theN-sulfate group. Subsequently, another six different enzymes (plus again sulfamidase) have to act, which ultimately leads to a complete degradation of the chain.
http://www.patient.co.uk/search.asp?searchterm=hunter+syndrome&searchcoll=All&x=9&y=15
http://www.mayoclinic.org/diseases-conditions/hunter-syndrome/basics/definition/con-20026538
http://en.wikipedia.org/wiki/Hunter_syndrome
Etymology
The syndrome is named after physician Charles A. Hunter (1873–1955), who first described it in 1917. Born in Scotland, Hunter emigrated to Canada and had a medical practice in Winnipeg, Manitoba.
http://en.wikipedia.org/wiki/Hunter_syndrome
Genetics and Risk factors
There are two major risk factors for developing Hunter syndrome:
- Family history:Hunter syndrome is caused by a defective chromosome, and a child must inherit the defective chromosome to develop the disease. Hunter syndrome is what's known as an X-linked recessive disease. This means that women carry the defective disease-causing X chromosome and can pass it on, but aren't affected by the disease themselves.
- Sex: Hunter syndrome nearly always occurs in males. Girls are less at risk of developing this disease because they inherit two X chromosomes. If one of the X chromosomes is defective, their normal X chromosome can provide a functioning gene. If the X chromosome of a male is defective, however, there isn't another normal X chromosome to compensate for the problem.
The IDS gene is situated on the telomere of the long arm of chromosome X at region Xq28. The gene has 9 exons and produces a transcript of 1.4 that encodes a precursor protein of 550 amino acide. More than 300 different mutations in the IDS gene had been reported in patients with Hunter syndrome including gene rearrangements caused by recombination with the IDS2 pseudogene, deletions of certain exons or the entire IDS gene or small mutations including insertions, deletions and point mutations that created a novel splice site.
More than 300 different mutations in the IDS gene had been reported in patients with Hunter syndrome (Human Gene Mutation Database; http://www.hgmd.org ). The mutational spectrum associated with the IDS gene is quite heterogeneous and ranges from point mutations to large-scale gene conversion or deletion. The majority of mutations are missense and nonsense mutation, and approximately 15% of mutations are presumed to be caused by a gross deletion.
For example,homology analyses revealed that arginine-88 is highly conserved among the human and eukaryotic sulfatases. The structure of human IDS was modeled by homology with crustal structure of human N-actyl-galactosamine-4-sulfatase (4S) and arysulfatase A (ASA). Therefore, residue 88 appears to be not essential for processing but important for IDS conformation. R88 residue is found adjacent to the active site residue, C84, and is a part of the core of the major domain of IDS. The alteration by proline, a more bulky hydrophobic residue, can affect the stability of the major domain structure.

Location of mutated residue (Arg88) in a tertiary structural model of IDS. The active site centre, Cys84 residue, is shown as green spheres and the other active site residues are shown as different spheres colors.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3115838/
http://www.patient.co.uk/search.asp?searchterm=hunter+syndrome&searchcoll=All&x=9&y=15
http://www.mayoclinic.org/diseases-conditions/hunter-syndrome/basics/definition/con-20026538
Signs and Symptoms
The symptoms of Hunter syndrome (MPS II) are generally not apparent at birth, but usually start to become noticeable after the first year of life. Often, the first symptoms of Hunter syndrome may include abdominal hernias , ear infections, runny noses, and colds.
Since these symptoms are quite common among all infants, they are not likely to lead a doctor to make a diagnosis of Hunter syndrome right away. As the buildup of GAG continues throughout the cells of the body, signs of Hunter syndrome become more visible.
There are two clinical manifestations of the genetic abnormality:
Type A - severe form with relentless progression towards profound mental retardation. It usually presents in late infancy and is progressive, leading to neurological impairment, deafness and somatic dysfunction, with death by adolescence/3rd decade.
Problems usually start before age 3, and common presenting features include:
* Delayed development, such as late walking or talking
* A broad nose and flared nostrils
* Claw-like hands
* A protruding tongue
* Coarsening of facial features
* Thickening of the lips, tongue and nostrils
* Decline in intellectual function
* Hearing problems
* Swollen and stiff joints
* Abdominal hernias
* Hepatosplenomegaly,resulting in a distended abdomen
Skin features:
* Pebble-like ivory-coloured papular skin lesions occur in a reticular pattern between the angles of the scapulae and the posterior axillary line, and over the pectoral area and lateral aspects of the upper arms and legs. The skin changes are virtually pathognomonic for the disease.
* The skin may also show hypertrichosis and excessive Mongolian spots.
Other features:
* Macrocephaly - common with a short trunk length compared to the extremities
* Short stature - develops gradually after the age of 3
* Flexion contractures
* Airways obstruction - from accumulation of heparan and dermatan sulfate in the trachea - including sleep apnea
* Cardiomyopathy and valvular abnormalities, eg aortic regurgitation - from cardiac infiltration
* Deafness - usually mixed sensorineural/conductive variety
* Abnormal retinal pigmentation and papilloedema - leading to visual impairment
* Carpal tunnel syndrome
Type B - mild form. This usually presents later and may not be noticed until adulthood. Life expectancy can be near-normal in this group, with relatively normal intellectual abilities but impaired reading and verbal skills. Some patients may only have involvement of one organ.
* Diagnosis often not made until later childhood or even adulthood
* Physical features are similar to those in type A but there is an absence of, or much less severe, neurocognitive involvement
* May also be dysplasia of the pelvis or femoral head and/or small carpal bones, and early osteoarthritis
* Life expectancy varies from 4th through to 7th decade
The age at onset of symptoms and the presence/absence of behavioural disturbances are predictive factors of ultimate disease severity in very young patients. Behavioral disturbances, that may occur in both forms of the illness, can often mimic combinations of symptoms of attention deficit hyperactivity disorder, autism, obsessive compulsive disorder, and/or sensory processing disorder, although the existence and level of symptoms may differ in each affected child. They often also include a lack of an appropriate sense of danger and aggression. The behavioral symptoms of Hunter syndrome generally precede neurodegeneration and often increase in severity until the mental handicaps become more pronounced.
http://www.mayoclinic.org/diseases-conditions/hunter-syndrome/basics/definition/con-20026538
http://www.nlm.nih.gov/medlineplus/ency/article/001203.htm
http://en.wikipedia.org/wiki/Hunter_syndrome
http://www.patient.co.uk/search.asp?searchterm=hunter+syndrome&searchcoll=All&x=9&y=15
Complications
A variety of complications can occur with Hunter syndrome depending on the type and severity of the disease. These may include:
- Respiratory complications.
All forms of MPS, including Hunter syndrome, involve respiratory complications that contribute to child's disability and sometimes cause death as the disease progresses. An enlarged tongue, thickened gums, and thickening of the nasal passages and windpipe (trachea) make breathing difficult. Children often have chronic ear and sinus infections, respiratory infections, and pneumonia. Sleep apnea, a condition in which breathing is intermittently interrupted during sleep, is often present because of airway constriction.
- Cardiac complications.
Thickening of tissue associated with Hunter syndrome can cause progressive thickening of the heart's valves. This causes improper closing of heart valves. As a result, the heart and other parts of the body don't receive blood efficiently. As the disease progresses, these conditions often become worse and typically result in heart failure.
The thickening of tissue can also cause narrowing of the aorta (coarctation) and other blood vessels. This in turn can result in high blood pressure (hypertension) and narrowing of arteries in the lungs (pulmonary hypertension).
- Skeletal and connective tissue complications.
The storage of undigested glycosaminoglycans in connective tissues results in abnormalities in bones, joints and ligaments. This reduces child's growth, causing pain and physical malformations, and making it difficult for him or her to move.
Nearly everyone with Hunter syndrome experiences joint stiffness, which makes movement painful. The stiffness is caused by swelling of joint connective tissues and abnormalities of cartilage and bones.
The group of abnormalities typically seen in the bones of people with Hunter syndrome is called dysostosis multiplex. Children with these abnormalities can develop irregularly shaped vertebrae and spines (kyphoscoliosis), ribs, arms, fingers, legs, and pelvises. Their skulls may press down on or fuse with their upper spines. These complications cause many people with Hunter syndrome to be abnormally short. Those with milder cases may reach normal or near-normal height.
Hernias (inguinal and umbilical) are common in Hunter syndrome. They happen because of problems with connective tissue. A hernia occurs when soft tissue, usually part of the intestine, pokes through a weak spot or tear in the lower abdominal wall. Hernias associated with Hunter syndrome can become quite large and are often one of the first signs of the disorder. Enlargement of the liver and spleen (hepatosplenomegaly), which is common in Hunter syndrome, may increase pressure in the abdomen, causing a hernia.
- Brain and nervous system complications.
A variety of neurological complications may be present and continue to develop in children with Hunter syndrome. Many neurological problems are caused by buildup of excess fluids in brain (hydrocephalus). Pressure from these fluids can cause other problems that may affect the eyes and other sensory organs, which can cause severe headaches, interfere with vision and change mental state. Placement of a shunt may help drain excess fluids and relieve pressure on the spinal cord. Imaging tests also may reveal a variety of cyst-like structures in parts of the brain.
The child also may develop a condition in which the membranes that surround the spinal cord may become thick and scarred (hypertrophic cervical pachymeningitis). This causes pressure and compression of the upper spinal cord. As a result, the child may develop fatigue in his or her legs and gradually weaken and become less physically active.
Other disorders, such as carpal tunnel syndrome, can result from nerve compression that happens because of bone deformities and storage of glycosaminoglycans in tissues.
http://www.mayoclinic.org/diseases-conditions/hunter-syndrome/basics/definition/con-20026538
Diagnosis
The visible signs and symptoms of Hunter syndrome (MPS II) in younger people are usually the first clues leading to a diagnosis. In general, the time of diagnosis occurs from about 2 to 4 years of age. Doctors may use laboratory tests to provide additional evidence that an MPS disorder is present, before making a definitive diagnosis by measuring the iduronate-2-sulfatase (I2S) enzyme activity. The most commonly used laboratory screening test for an MPS disorder is a urine test for GAG. It is important to note that the urine test for GAG can occasionally be normal and yet the child still may have an MPS disorder. A definitive diagnosis of Hunter syndrome is made by measuring I2S activity in serum, white blood cells, or fibroblasts from skin biopsy. In some people with Hunter syndrome, analysis of the I2S gene can determine clinical severity. Prenatal diagnosis is routinely available by measuring I2S enzymatic activity in amniotic fluid or in chorionic villus tissue.
http://en.wikipedia.org/wiki/Hunter_syndrome
Treatments and drugs
Emerging treatments
Although there's no cure for Hunter or other MPS syndromes, some treatments that are in their early stages have had some success by slowing the disease's progress and lessening its severity.
These emerging treatments include:
- Bone marrow transplantation.
For a long time, the most efficient approach had been to use bone marrow graft, emerging into hematopoietic stem cell transplantation. Based upon the same theory, they each have the advantage of procuring a new source of the missing I2S. This treatment can help ease the problems of breathing, mobility, and heart, liver and spleen function. It can also help prevent mental regression. This treatment won't help with bone or vision problems.
- Enzyme therapy.
This treatment uses man-made or genetically engineered enzymes to replace child's missing or defective enzymes and ease the disease symptoms. Called idursulfase (Elaprase), this treatment is given once a week through an intravenous line. Given early enough, enzyme replacement therapy may delay or prevent some of the symptoms of Hunter syndrome. It's unclear, however, if the improvements seen with this therapy are significant enough to raise quality of life for people with the disease. In addition, benefits in thinking and intelligence haven't been seen with enzyme replacement therapy.
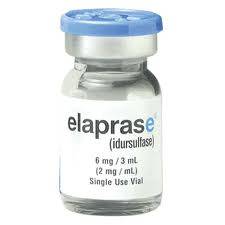
Idursulfase, a purified form of the lysosomal enzyme iduronate-2-sulfatase produced by recombinant DNA technology in a human cell line which underwent clinical trial in 2006 was approved by the United States Food and Drug Administration as an enzyme replacement treatment for Hunter syndrome.
- Gene therapy.
Replacing the chromosome responsible for producing the missing enzyme could theoretically cure Hunter syndrome, but much more research is needed.
Treatments for complications
- Relief for respiratory complications.
Removal of tonsils and adenoids can open up airway and relieve sleep apnea. But as the disease progresses, tissues continue to thicken and these problems can come back. Breathing devices that use air pressure to keep the airway open — such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) devices — can help with upper airway obstructions and sleep apnea. Keeping airway open can also help avoid low blood oxygen levels (hypoxemia).
- Addressing heart complications.
If the child has severe cardiovascular problems, it could be necessary surgery to replace heart valves.
- Treatment for skeletal and connective tissue problems.
Because most children with Hunter syndrome don't heal well and often have complications after surgery, options are limited for addressing skeletal and connective tissue complications. For example, surgery can stabilize the spine using internal hardware but it is difficult when bones are fragile.
Joint flexibility can be improved with physical therapy, which helps address stiffness and maintain function. However, physical therapy can't stop the progressive decline of joint motion.
Surgery can repair hernias, but because of weakness in connective tissues, results usually aren't ideal. The procedure often needs to be repeated. One option is to manage hernias with supportive trusses rather than surgery because of the risks of anesthesia and surgery.
- Managing neurological complications.
Problems associated with the buildup of fluid and tissue around the brain and spinal cord are difficult to address because of the inherent risks in treating these parts of the body. Thanks to surgery it's possible to drain excess fluids or remove built-up tissue.
http://www.mayoclinic.org/diseases-conditions/hunter-syndrome/basics/definition/con-20026538
http://en.wikipedia.org/wiki/Hunter_syndrome
Prognosis
Death is usually as a result of cardiorespiratory complications. Severe variant sufferers have average onset 2.5 years with an average age of death of ~12 years - but some may survive into their thirties. Mild variant sufferers have an average age of onset of 4.3 years with average age of death 21.7 years - but some may survive into their fourth decade and beyond. Cognitive impairment is associated with reduced life expectancy.
http://www.patient.co.uk/search.asp?searchterm=hunter+syndrome&searchcoll=All&x=9&y=15
Epidemiology
There are estimated to be approximately 2,000 people afflicted with Hunter Syndrome worldwide, 500 of whom live in the United States. There are about 30 Hunter Syndrome patients in Canada. There are 2 Hunter Syndrome patients in New Zealand. There are 6 Hunter Syndrome patients in Ireland, at least 1 case in Iran, 1 case in Saudi Arabia, 1 case in Chile, 1 case in Pakistan, 1 case in the Philippines 1 case in the West Bank (Israel). 70 Hunter Syndrome patients in Korea. There is one case in the city of Kolkata, West Bengal, India as broadcast by a regional television channel.20 cases in Poland.
A study in the United Kingdom indicated an incidence among males of approximately 1 in 130.000 male live births.
http://en.wikipedia.org/wiki/Hunter_syndrome
Notable cases
On July 24, 2004, Andrew Wragg, 38, of Worthing, West Sussex, England, suffocated his 10 year old son Jacob with a pillow, because of the boy's disabilities related to Hunter syndrome. On December 13, 2005 Andrew Wragg walked out of Lewes Crown Court a free man after a jury determined that he did not murder his 10-year-old son, who was diagnosed with Hunter Syndrome. A military security specialist, Wragg also claimed that he was under stress after returning from the war in Iraq. He denied murdering Jacob, but pleaded guilty to manslaughter by reason of diminished capacity. Mrs. Justice Anne Rafferty, calling the case "exceptional", gave Wragg a two-year prison sentence for manslaughter, then suspended his sentence for two years. Rafferty said there was "nothing to be gained" from sending Wragg to prison for the crime.
http://en.wikipedia.org/wiki/Hunter_syndrome
See also