Giordani Ilaria
Valentini Letizia
DEFINITION
Euthyroid Sick Syndrome (or Low T3 Syndrome or Non-Thyroidal Illness Syndrome) is a condition of abnormal thyroid hormones release in patients with apparently normal thyroid gland during severe systemic illness, physical trauma, and psychiatric disturbances. The most common abnormality results in low T3 thyroid hormone with progressive decrease in thyroxine (T4) and TSH. The fact that the syndrome is not caused by an intrinsic abnormality in thyroid function has lead to the definition of “Non-Thyroidal Illness Syndrome”.
T3 is the biologically active thyroid hormone and its low serum levels in critical illness reflect altered thyroid homeostasis and a mechanism of adaptation. Such changes may be a self-protective adaptation to illness, as the body attempts to conserve energy.
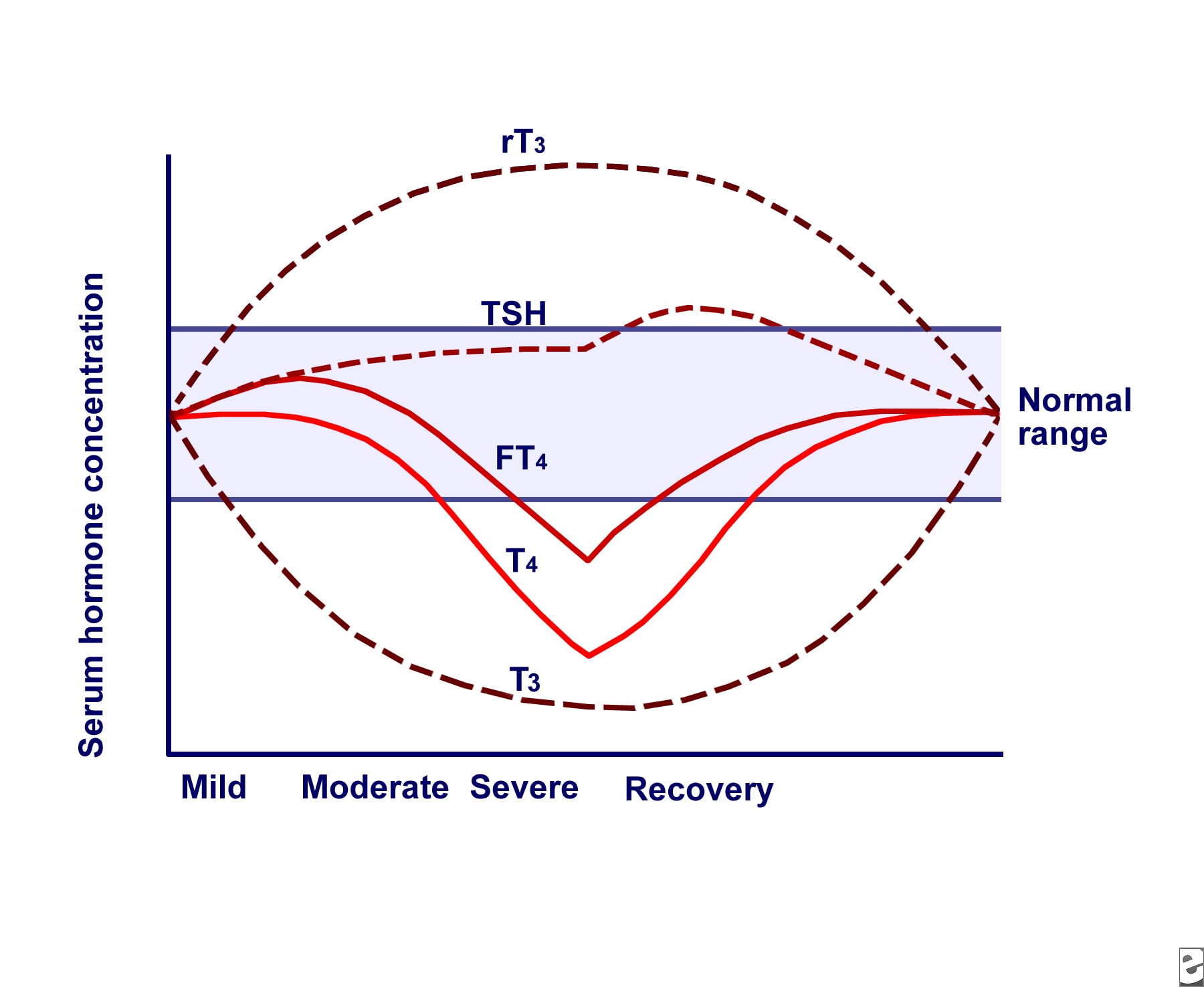
The most prominent alterations are low serum triiodothyronine (T3) and elevated reverse T3 (rT3), leading to the general term "low T3 syndrome." Thyroid-stimulating hormone (TSH), thyroxine (T4), free T4 (FT4), and free T4 index (FTI) also are affected in variable degrees based on the severity and duration of the non-thyroidal illness. As the severity increases, both serum T3 and T4 levels drop and gradually normalize as the patient recovers. After recovery from an NTI, these thyroid function test result abnormalities should be completely reversible.
EPIDEMIOLOGY
In patients with no previous diagnosis of thyroid disease, critical illness (defined as a life-threatening condition) can cause profound changes in thyroid hormone metabolism.
Causes of euthyroid sick syndrome include a number of acute and chronic conditions, including pneumonia, fasting, starvation, anorexia nervosa, sepsis, trauma, cardiopulmonary bypass, malignancy, stress, heart failure, hypothermia, myocardial infarction, chronic renal failure, cirrhosis and diabetic ketoacidosis.
Euthyroid sick syndrome affects up to 70% of patients hospitalized with diseases of various etiologies, especially in ICUs. This changes in parameters of thyroid function are rarely isolated. They are often associated with alterations in other endocrine axes, in particular reduction in serum gonadotropin and sex hormone concentrations and increase in serum free cortisol levels.
THYROID HORMONES
See also: Thyroid Hormones
Thyroid hormones (T4 and T3) are produced by the follicular cells of the thyroid gland and are regulated by TSH made by the thyrotropes of the anterior pituitary gland.

In peripheric tissues T4 is converted as required by iodothyronine deiodinase. T3 is more active than T4 and is the final form of the hormone, though it is present in less quantity than T4.
When dietary iodine is sufficient, the major product of the thyroid gland is thyroxine (T4) which is secreted at a rate of 10-fold that of 3,5,3′-triiodothyronine (T3) in humans.
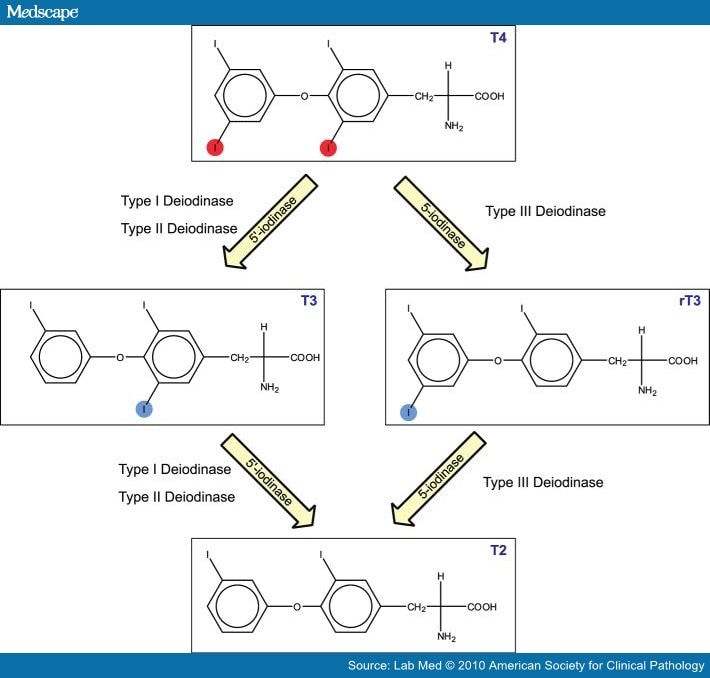
But a rate-limiting step in thyroid hormone action is the conversion of the prohormone T4 to T3. This is the role of type 1 and 2 iodothyronine deiodinases (D1 and D2). While the half-life of T4 in humans is about 1 week, that of T3 is much shorter, <24 h, and its inactivation in peripheral tissues by removal of an inner ring iodine from T3 is primarily due to the action of type 3 iodothyronine deiodinase (D3). These are the characteristic of the selenodeiodinases:

The function of thyroid hormones are various:
- increase the basal metabolic rate
- increase HR and cardiac output
- potentiate the effects of catecholamines by increasing the body's sensitivity
- regulate long bone growth and brain development (and are essential for the development and differentiation of all cells of the human body)
- regulate metabolism of proteins, fat and carbohydrates
SYMPTOMS
Symptoms are non-specific, ranging from asymptomatic conditions to symptoms of hypothyroidism. In most cases sick patients with low serum T3 are often regarded as being clinically euthyroid (from which the name “Euthyroid sick syndrome”). Also, the symptoms associated with the underlying disease are predominant and the diagnosis is based only on laboratory tests.
DIAGNOSIS
The diagnosis is based on the evaluation of serum TSH and serum fT3/fT4 and on the clinical examination. The abnormality observed include low serum levels of T3, normal or low serum levels of T4 and normal or low serum levels of TSH. Is important to consider that thyroid function should not be assessed in seriously ill patients unless there is a strong suspicion of thyroid disfunction. In this case, measurement of serum TSH alone is inadequate for the evaluation of thyroid function. When the evaluation suggests central hypothyroidism, is important to know that the probability of euthyroid sick syndrome is much higher than the pituitary or hypothalamic disease.
The differential diagnosis is with primary hypothyroidism. The best test is measurement of TSH, which in euthyroid sick syndrome is low, normal, or slightly elevated but not as high as it would be in hypothyroidism. Serum rT3 is elevated, although this measurement is rarely done. Serum cortisol is often elevated in euthyroid sick syndrome and low or low-normal in hypothyroidism due to pituitary-hypothalamic disease.
| Euthyroid Sick Syndrome | Primary hypothyroidism |
| fT3 | low | normal/low |
| fT4 | normal/low | low |
| TSH | normal/low | high |
| r-T3 | high | low |
Also, it is necessary to consider the possible interactions of the drugs in use with the metabolism of thyroid hormones. In fact, other than the drugs that can cause alteration in thyroid function (amiodarone, radiographic agents, thionamides) or that decrease LT4 absorption (PPI, colestyramine), there are many drugs that can cause alterations in thyroid parameters without thyroid disfunction. These include many drugs of common use, such as glucocorticoids, heparin, NSAIDs, furosemide and others.
PATHOGENESIS
There are different mechanisms underlying the euthyroid sick syndrome:
- Alterations in hypothalamic-pituitary axis. Serum TSH is often normal/low despite the fact that circulating T3 is low. It seems that the low TSH associated with critical illness arises from a central hypothyroidism caused by both prolonged diminished calorie intake and release of inflammatory cytokines.
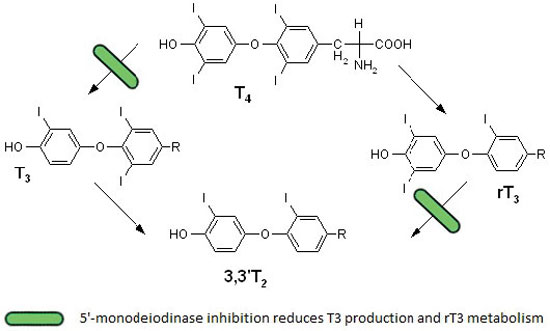
- Alterations in the peripheral conversion of T4 to T3. In illness the extra-thyroidal conversion of T4 to T3 is diminished due to a diminution in function in iodothyronine deiodinases, especially type I. It also leads to an increase in reverse T3, due to decreased clearance by deiodinase, as shown in the picture below.
Additionally, many drugs commonly used in these cases also reduce the conversion of T4 to T3.
See also: Deiodinase
- Alterations in thyroid hormone-binding proteins. In severe illness, the concentration of binding proteins may be changed as a consequence of the acute phase response.
- Impaired uptake of thyroid hormone by peripheral tissues.
- Diminished expression of ligand-regulated transcription factors, which are responsible for thyroid hormone actions.
Mechanisms behind the non-thyroidal illness syndrome: an update. 2010
There are many conditions that can lead to an increase in reverse T3 levels due to alterations in peripheral conversion of thyroid hormones:
COMPLICATIONS
Euthyroid sick syndrome has commonly been interpreted as an adaptive compensatory and thus beneficial response that decreases energy consumption in diseased states. This interpretation, however, has recently been questioned, and many studies have shown how patients affected by euthyroid sick syndrome have an increased risk of death, regardless of their underlying disease.
ESS is very common in acutely ill, hospitalized older patients, and its presence, beside the specific underlying disease, is characterized by an advanced disease state, an increased level of acute inflammation indexes and a significantly higher cumulative death rate.
Consequently, ESS is considered as the most sensitive independent predictor of short-term survival in acutely ill hospitalized older patients, particularly when associated with elevated serum inflammation indexes.
Non-thyroidal illness syndrome and short-term survival in a hospitalised older population. 2010
Also, euthyroid sick syndrome has been found in patients affected by NSCLC, and was found to be correlated with disease stage and weight loss; it follows that the presence of ESS can be used as a predictor of poor prognosis in NSCLC patients.
Nutritional and prognostic significance of sick euthyroid syndrome in non-small cell lung cancer patients. 2008
Reduced fT3 levels were found in most patients with respiratory failure due to respiratory disorders. As it was found that plasma levels of fT3 were related to clinical status and pulmonary gas exchange impairment, and the normalization of fT3 levels was associated with an improvement in gas exchange, it has been suggested that fT3 levels may be a reliable predictor of clinical outcome.
Moreover, in patients undergoing cardiac surgery, fT3 levels correlate with the time spent in intensive care unit, and they can thus be taken as an index of the overall clinical outcome.
A recent report has found a strong correlation between low T3 state and the long-term prognosis in patients with various cardiovascular disorders.
Low triiodothyronine (T3) state: a predictor of outcome in respiratory failure? Results of a clinical pilot study. 2004
Euthyroid sick syndrome has been described in patients with acute myocardial infarction and heart failure, and in adults and children after cardiopulmonary bypass. It has been shown that low T3 concentrations represent a strong independent predictive marker of poor prognosis in cardiac patients and might represent a determinant factor directly implicated in the evolution and prognosis of these patients.
Low-T3 syndrome: a strong prognostic predictor of death in patients with heart disease.
2003
In addiction, a study has examinated thyroid hormones levels in burn patients admitted to the Burn Center of Turin: they have shown that fT3 and TSH levels were significantly lower (p<0.0002) in non-survivors compared to survivors.
Low triiodothyronine serum levels as a predictor of poor prognosis in burn patients. 2008
THERAPY
Since many studies have shown that the presence of euthyroid sick syndrome is associated with increased mortality and poor prognosis in critically ill patients, would seemed indicated thyroid hormone replacement therapy.
Indeed, only a few studies have examined the use of supplemental T4 therapy in these patients, and there was no significant difference in mortality.
It could be debated that levo-thyroxine therapy in the sick euthyroid syndrome would be unlikely to have any effect because of the pronounced inhibition of conversion of T4 to T3. Therefore some studies have examined the effect of treatment with T3 in critically ill patients: treatment normalized serum T3 concentrations but resulted in no change in either mortality or basal metabolic rate.
At this moment, thyroid hormone treatment is not recommended in euthyroid sick syndrome, but further studies are required to determine whether is necessary the supplementation, which thyroid hormone is best to use, and to define the optimal dose.