The correlation between Microbiota and Cancer
Introduction
The human gut harbors a complex community of microbes, collectively called microbiota.
Recent research has revealed many aspects of our health that are affected by intestinal microbiota. For instance, gut microbes can influence both local and body-wide immune system activity and inflammation.

In their intestine, humans possess an “extended genome” of millions of microbial genes—the microbiome. Because this complex symbiosis influences host metabolism, physiology, and gene expression, it has been proposed that humans are complex biologic “superorganisms.” Advances in microbiologic analysis and systems biology are now beginning to implicate the gut microbiome in the etiology of localized intestinal diseases such as the irritable bowel syndrome, inflammatory bowel disease, and colon cancer.
These approaches also suggest possible links between the gut and previously unassociated systemic conditions such as type 2 diabetes and obesity.
The elucidation of the intestinal microbiome is therefore likely to underpin future disease prevention strategies, personalized health care regimens, and the development of novel therapeutic interventions.
Impact of pelvic radiotherapy on gut microbiota of gynecological cancer patients revealed by massive pyrosequencing,2013
The human gut microbiome, 2008
Microbiota in cancer therapy
Given that microbiome is "the ecological community of commensal, symbiotic, and pathogenic microorganisms that literally share our body space" the point is now to highlight how the effectiveness of certain cancer therapies may depend, according to a study in mice, on microbes that live in the intestine.
The findings suggest that antibiotics used to treat infections might hinder the effects of anti-cancer therapies.
Some cancer therapies work by stimulating anti-cancer immune responses. To investigate whether gut microbes can affect cancer treatments, scientists at NIH’s National Cancer Institute (NCI) studied germ-free mice, raised in sterile conditions from birth. These mice harbor no bacteria.
The team also studied conventionally raised mice given a potent antibiotic cocktail in their drinking water beginning 3 weeks prior to the experiments.
Lymphoma, colon, and melanoma cancer cells were injected under the skin of the mice. The cells formed tumors that grew to a diameter of one-fifth of an inch or more. The tumors were then treated with either an immunotherapy that included CpG-oligonucleotides or with the mainstay chemotherapy drugs oxaliplatin and cisplatin. The immunotherapy stimulates an immune attack on cancer cells, whereas the chemotherapy drugs directly damage tumors.
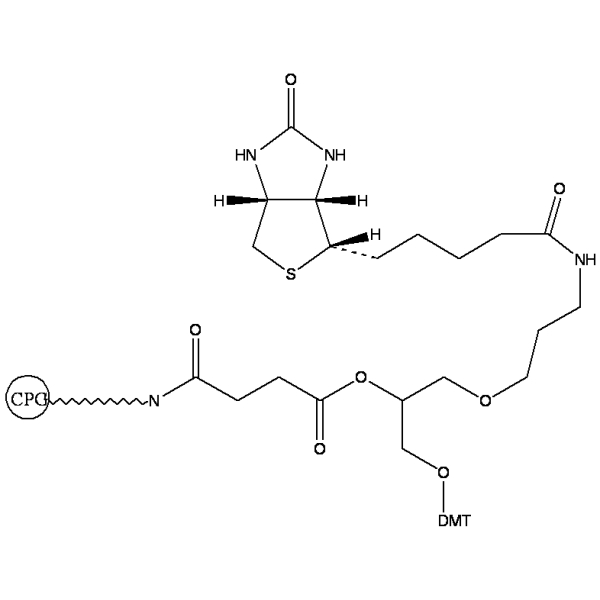 CpG-oligonucleotide
CpG-oligonucleotide
 oxaliplatin
oxaliplatin
 cisplatin
cisplatin
The researchers found that tumors responded poorly to the immunotherapy in both germ-free mice and mice that received the antibiotic cocktail. The tumors in these mice also responded poorly to oxaliplatin and cisplatin.
Further research showed that the mice produced lower levels of immune signaling molecules called cytokines after treatment than control mice.
The germ-free and antibiotic-treated mice also had reduced expression of genes involved in inflammation.
Recent studies have shown that individuals with colorectal cancer have an altered gut microbiome compared to healthy controls. It remains unclear whether these differences are a response to tumorigenesis or actively drive tumorigenesis.
To determine the role of the gut microbiome in the development of colorectal cancer, the gut microbiome has been characterized in a murine model of inflammation-associated colorectal cancer that mirrors what is seen in humans. Then the development of an abnormal microbial community structure associated with inflammation and tumorigenesis in the colon has been followed.
Tumor-bearing mice showed enrichment in operational taxonomic units (OTUs) affiliated with members of the Bacteroides, Odoribacter, and Akkermansia genera and decreases in OTUs affiliated with members of the Prevotellaceae and Porphyromonadaceae families. Conventionalization of germfree mice with microbiota from tumor-bearing mice significantly increased tumorigenesis in the colon compared to that for animals colonized with a healthy gut microbiome from untreated mice.
Furthermore, at the end of the model, germfree mice colonized with microbiota from tumor-bearing mice harbored a higher relative abundance of populations associated with tumor formation in conventional animals.
Manipulation of the gut microbiome with antibiotics resulted in a dramatic decrease in both the number and size of tumors. The results demonstrate that changes in the gut microbiome associated with inflammation and tumorigenesis directly contribute to tumorigenesis and suggest that interventions affecting the composition of the microbiome may be a strategy to prevent the development of colon cancer.
Clinical identification of bacteria in human chronic wound infections: culturing vs. 16S ribosomal DNA sequencing,2012
Gut Microbes and Cancer,2013
Perturbation of microbiota promotes cancer developing
The balance and the state of homeostasis and symbiotic relationships is maintained by the separation of microbial entities from the host through a multi-level barrier, by a eubiotic microbiome that actively suppresses pathobionts and that maintains a symbiotic relationship with the host, and by a state of low inflammation in the host.
The benefits of gut microbiota are clear, therefore a perturbation of his balance leads to chain reactions that ultimately result in a cancer-promoting state with a failing barrier, inflammation and dysbiosis.
This state includes qualitative and sometimes quantitative changes in the microbiota, as we can see in Picture 3, these are: failure of the barrier either physically (for example, at the level of tight junctions or at the mucous layer) or at the level of antibacterial defence systems — either those of epithelial cells or those of cells from the gut-associated lymphoid tissue (GALT); and increased inflammatory responses, which are often mediated by pattern recognition receptors (PRRs) and downstream cytokines that promote epithelial cell proliferation and survival.

The Microbiome and Cancer;2013
Molecular Pathways
It is very important to point out the molecular mechanisms through which the bacterial microbiome promotes carcinogenesis.
To better understand these processes we must underline 3 main points (clearly represented in the next picture).
- Changes in the microbiome and host defences may favour increased bacterial translocation, leading to increased inflammation, which is mediated by microorganism-associated molecular patterns (MAMPs) that activate Toll-like receptors (TLRs) in several cell types, including macrophages, myofibroblasts, epithelial cells and tumour cells. These effects may occur locally or through long-distance effects in other organs.
- Genotoxic effects are mediated by bacterial genotoxins, such as colibactin and cytolethal distending toxin (CDT), that, after being delivered to the nucleus of host cells, actively induce DNA damage in organs that are in direct contact with the microbiome, such as the gastrointestinal tract. Reactive oxygen species (ROS) and reactive nitrogen species (RNS) released from inflammatory cells such as macrophages, as well as hydrogen sulphide (H2S) from the bacterial microbiota, may also be genotoxic.
- Metabolic actions of the microbiome may result in the activation of genotoxins such as acetaldehyde, dietary nitrosamine and other carcinogens, in the metabolism of hormones such as oestrogen and testosterone, in the metabolism of bile acids and in alterations of energy harvest.
The microbiota also mediates tumour suppressive effects (shown in green) through inactivation of carcinogens, through the generation of short-chain fatty acids such as butyrate and through the biological activation of cancer-preventing phytochemicals.
Many of these tumorigenic and tumour-suppressive mediators exert both local and long-distance effects.

The gut flora as a forgotten organ,2006
The microbiome and cancer,2013
Treatments
Understanding the normal temporal variation in the human microbiome is critical to developing treatments for putative microbiome-related afflictions such as obesity, Crohn's disease, inflammatory bowel disease, malnutrition and most of all colon cancer. Sequencing and computational technologies, however, have been a limiting factor in performing dense time series analysis of the human microbiome.
The largest human microbiota time series analysis to date, covering two individuals at four body sites over 396 timepoints found that despite stable differences between body sites and individuals, there is pronounced variability in an individual's microbiota across months, weeks and even days.
Additionally, only a small fraction of the total taxa found within a single body site appear to be present across all time points, suggesting that no core temporal microbiome exists at high abundance (although some microbes may be present but drop below the detection threshold). Many more taxa appear to be persistent but non-permanent community members.
Scientist are targeting the bacterial microbiota for therapeutic modulation of carcinogenesis.
Nowadays the most efficient therapies to contrast the dysbiosis or the increased translocation of microbiota that may stimulate carcinogenic effector mechanisms, are antibiotics targeting against specific microorganism.
Useful are also prebiotics, which might reinforce the correct intestinal flora, and drugs targeting genotoxins or bacterially-induced inflammation.
Genetically modified microbiota has, also, been sperimented on many patients and has given significant results.
Although, the last therapeutic frontier accounted for, is microbiome transplant. This consists in a selective transplant of specific bacteria and microorganism that help to re-establish homeostasis and microbiome balance.
An interesting application of microbiome transplant is the treatment of Clostridium difficile infection (CDI).
The current standard of care for Clostridium difficile infection (CDI) is antibiotic treatment. However, approximately 20% to 30% of the patients experience a recurrence in symptoms following initial antimicrobial treatment. Approximately 45-65% of patients with a first recurrence develop persistent recurrent CDI. Persistent recurrent CDI is associated with high morbidity and mortality.
A major problem with antibiotic therapy is that it disrupts the normal fecal microbiota, allowing Clostridium difficile to colonize the gut. Restoration of colonization resistance is necessary to break the cycle of recurrence.
This once again shows how important is to maintain the correct balance of gut microbioma and opens the doors to what has been defined “microbiome transplantation”.
In this specific case the treatment of Clostridium difficile infection (CDI) consists of a new and revolutionary approach consisting in Fecal Transplantation and Microbiota Restoration.
Fecal transplantation (FT) is a non-pharmacological treatment option for recurrent CDI that restores the fecal microbiome and colonization resistance.
Fecal Transplantation has been used successfully for more than 50 years for the treatment of recurrent CDI. Over 480 cases of FT have been reported with an approximately 90% cumulative success rate in curing recurrent CDI without any adverse events attributable to the FT material itself.
Although studies have demonstrated high patient acceptance of FT, the processes involved in screening donors and preparing the fecal material for transplantation are labor intensive and cumbersome to implement in normal clinical practice. Use of the therapy has, therefore, been limited to a few centers with limited capacity to treat the large number of patients in need of an effective treatment for recurring Clostridium Difficile Infection.

Moving pictures of the human microbiome,2011
Butyrate and human colon
Butyrate, also known as butanoate, is the traditional name for the conjugate base of butyric acid. The formula of the butyrate ion is C4H7O2−.
Sodium butyrate, a naturally occurring short fatty acid, is present in the human large bowel in millimolar amounts as a result of bacterial fermentation of dietary fibre.
Sodium butyrate (NaB), is able to induce cell cycle arrest, differentiation and apoptosis in colon cancer cells.
In addition to these it also has an effect on two angiogenesis-related proteins in a colon carcinoma cell line: vascular endothelial growth factor (VEGF), the most potent angiogenic factor, and hypoxia-inducible factor (HIF)-1alpha, the main transcription activator of the VEGF gene, which are both constitutively expressed at high levels in HT29 also in normoxic conditions.
This indicate that NaB, besides regulating other fundamental cellular processes, is able to modulate the expression of two important angiogenesis-related molecules and suggested a further possible clinical application of this short-chain fatty acid as an anti-angiogenic compound in association with conventional chemotherapeutic agents.
Tumorigenesis of gastric cancer is closely related to unlimited cellular proliferation, poor differentiation, and deregulated apoptosis of gastric mucosa epithelial cells under different pathogenic factors.
Thus, it is important to correct this unbalanced status using proper methods to reduce the incidence of gastric tumor. Studies have shown that butyric acid, a product of dietary fiber fermentation in the colon, could provide energy for normal colonic mucosal epithelial cells and maintain their renewal.
Sodium butyrate can promote proliferation in normal colonic epithelial cells and it is known that proliferation of intestinal mucosal epithelium could be a precancerous.
Some researchers suggest that diet fibers may increase the risk of colon cancer. Studies have revealed different biological effects of sodium butyrate on tumor cells compared with on normal cells.
On the other hand, normal colon epithelial cells could effectively catabolize sodium butyrate to provide energy for themselves, thus reduce the inhibitory effect of sodium butyrate on cell growth.
Once the normal colon cells undergo carcinogenesis, normal metabolism of sodium butyrate may get lost, which allows this compound to exert its anti-tumor effect in tumor cells.
It is also suggested that the anti- proliferation effect of sodium butyrate is tumor-specific.
Currently, most reports on the anti-tumor effect of sodium butyrate are focused on colon cancer. However, there are few studies describing its anti-tumor effect on gastric cancer.
Sodium butyrate induces apoptosis in human colonic tumour cell lines in a p53-independent pathway: Implications for the possible role of dietary fibre in the prevention of large-bowel cancer, 2006
Butyrate production from dietary fibre and protection against large bowel cancer in a rat model, 1993
Conclusions
DNA sequencing and computational advances provide the ability to go beyond infrequent snapshots of our human-associated microbial ecology to high-resolution assessments of temporal variations over protracted periods, within and between body habitats and individuals. This capacity will allow to define normal variation and pathologic states, and assess responses to therapeutic interventions.
As more attention is paid to viewing ourselves as a supraorganism, comprising interacting microbial and human cellular and genetic components, it is apparent that much more precise understanding is needed of what constitutes normal temporal variations in our microbial community structures and functions.
Variation in the human microbiome within and between our various body habitats, lifecycle stages, and cultural settings is largely unexplored.
High-resolution time series studies provide a foundation for discriminating between 'normal' perturbations and pathologic states, and between organisms that are simply passing through a body habitat or are entrenched residents of an ecosystem.
Similarly, these types of studies are needed to understand the immigration and emigration patterns of microbes between our body sites, between cohabitating individuals, and between ourselves and the myriad of environments we contact on a daily basis.
The importance of microbiome for our body functions is acknowledged, but research has still to make it’s course and produce the right answers that may lead in the near future to manipulate gut microbioma to treat different pathologies including colon cancer.
Scientists publishes first human microbiome analysis,2006