Down's Syndrome
Down’s Syndrome or Trisomy 21 is the best known chromosomal diseases and is the most common genetic cause of modern mental retardation.
Down's Syndrome is one of three well-defined chromosomal diseases, in which there is trisomy of an entire chromosome (trisomy 21, trisomy 18, trisomy 13) compatible with the post-natal life.
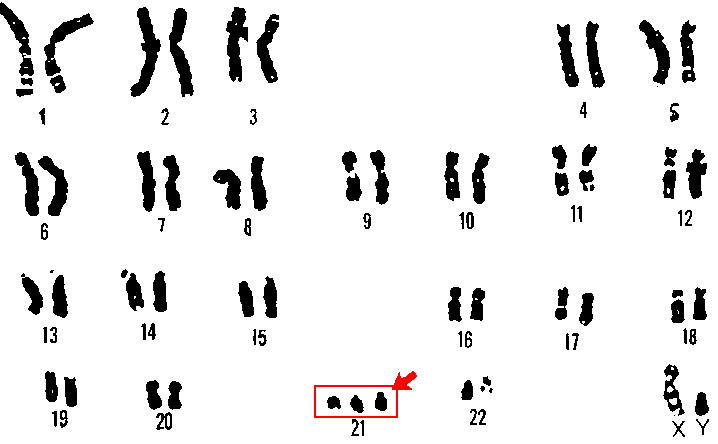
| Karyotype of an infant with Down's Syndrome,in which is highlighted the Trisomy 21 |
The syndrome has been clinically described for the first time in 1866 by Langdon Down (from which it takes its name), but his cause was a deep mystery for nearly a century.
Some features of its distribution in the population have attracted attention:
a) maternal age increased,
b) concordance in monozygotic twins,
c) an almost complete discordance in heterozygous twins and other family members.
Although since the '30s had been suggested as an abnormal chromosome could explain these observations, only in 1959 it was established that the majority of children born with this syndrome possessed 47 chromosomes, for the presence of an extra chromosome 21.
Although the chromosomal basis of the syndrome are clear, the reason chromosomal anomaly is still not understood. One possibility is the model of the "Old Egg", more old the oocyte is more much more is inceased the possibility of non-disjunction. A feature of this model is that the causative event leading to the emergence today of a sick child can be placed 35 or 40 years before, when the child's mother had them stesee a fetus.
This syndrome can be detected prenatally by cytogenetic analysis of chorionic villi or amniotic fluid cells and in 80% of cases prenatal diagnosis are eseguitee because the mother's age is advanced.
Down syndrome is usually *diagnosed at birth*due to its dysmorphic features that, while varying from patient to patient, producing a specific phenotype.
The characteristic facies, with a round face with a flat profile and a short nose with flat root, ears small and round with a small lobule and adhering to eyerims oblique from top to bottom and from outside to inside, the skin fold at the level of inner corner of the eye (epicanthus) iris features with white spots arranged to form a radial crown, called Brushfield spots.
The mouth is small, the teeth are small and irregular and the language is great (macroglossia).
The skull is small and has a flattened occipital; fountains are wide and close late than normal.
The neck is short, broad and flat and the overlying skin is thickened. On the palm of the hand can be a single transverse groove. The metacarpals and phalanges have length less than the norm, in particular the middle phalanx of the 5th finger, which has a single fold of flexion.
Mental retardation becomes apparent towards the end of the first year of age and IQ is normally between 30 and 60.
There are three types of chromosomal abnormalities responsible for Down syndrome:
1) Trisomia Free
This is the most common chromosomal abnormality (80 of cases) and consists in all cells of the body three 21 chromosomes instead of two. This condition is caused by meiotic nondisjunction of chromosome 21 in one of two gametes (90 of cases during meiosis I of maternal egg cell, 10 % during meiosis II paternal sperm).
2) Trisomy by Translocation
Corresponds to 18% of cases. The chromosome 21 (or a part of it) is joined to another chromosome (usually 14 or 22). The translocation of chromosome 21 to another chromosome can be totally random (80 % of cases), or it can result from a condition already present in one of the parents.
3) Mosaicism
More rarely seen, this condition requires the presence in the body of the person with the syndrome of both normal cells with 46 chromosomes and cells with 47 chromosomes, with different percentages of the two cell lines. It is assumed that This situation results from a mutation occurred in some cells of the embryo during the early stages of development.
The final effect of the three chromosomal abnormalities is still the same: in the cells of various organs of chromosome 21 is present in triplicate, by configuring the Down syndrome.

| The table shows how the rise in maternal age is correlated with the increase in the chance of having children with Down's syndrome. |
The incidence in the population is 1/800. Around 30 years, the risk begins to rise sharply, reaching 1/25 for very high maternal age .
Furthermore, the risk of the syndrome due to translocation or partial trisomy is not related to maternal age, at last paternal age meter seems to have no influence on risk.
Down's syndrome
Fluoxetine
Fluoxetine (also known by the tradenames Prozac, Sarafem, Ladose and Fontex) is an antidepressant of the selective serotonin reuptake inhibitor (SSRIs) class.

| 3D structure of Fluoxetine (Blue = Nitrogen, Orange = Fluorine, Red = Oxygen) |
Fluoxetine was first documented in 1974 by scientists from Eli Lilly and Company and final approval to market the drug in December 1987. Fluoxetine went off-patent in August 2001.
Fluoxetine is approved for the treatment of major depression (including pediatric depression), obsessive-compulsive disorder (in both adult and paediatric populations), bulimia nervosa, panic disorder and premenstrual dysphoric disorder.
In 2010, over 24.4 million prescriptions for generic formulations of fluoxetine were filled in the United States, making it the third most prescribed antidepressant.

| The mechanism of an inhibitor of serotonin reuptake inhibitors (SSRIs), such as Fluoxetine |
Fluoxetine's mechanism of action is predominantly that of a serotonin reuptake inhibitor.
Fluoxetine does not directly stimulate the production of new Serotonin, but inhibit the presynaptic reuptake and its elimination in the intestines are accumulating over time until restoration of normal values.
Pre-clinical studies conducted on animals have shown that therapeutic doses of antidepressants serotonin reuptake inhibitors (SSRIs) have proven quite safe because they don't increase the risk of teratogenicity and fetal malformation.
In particular, in experiments with Fluoxetine has not been reported malformation in rats and rabbits, even at doses 10 times higher than the MRD (Maximum Recommended Dose).
Fluoxetine
Fluoxetine and pregnancy
Prenatal pharmacotherapy, using Fluoxetine, rescues brain development in a Down’s Syndrome mouse model
In December 2013 a research group of the Department of Biomedical and Neuromotor Sciences of Bologna's University, led by Renata Bartesaghi, published in the journal of neuroscience "Brain" a study that demonstrates the possibility of being able to recover, on a specific model of laboratory mouse, the development of the brain affected by Down's Syndrome, thanks to a drug therapy prenatal.
Many evidence shows that widespread neurogenesis impairment is a major determinant of abnormal brain development and, hence, of intellectual disability, that is a strongly disabling feature, in Down's syndrome. This defect is worsened by dendritic hypotrophy and connectivity alterations.
Most of the pharmacotherapies designed to improve cognitive performance in Down’s syndrome have been attempted in Down’s syndrome mouse models during adult life stages.
This research is innovative because it highlights, for the first time, how it is possible to correct in the laboratory, before birth, the brain changes and cognitive disabilities caused by Down syndrome.
Correction of neurogenesis during the very first stages of brain formation may, in turn, rescue improper brain wiring. Infact, with the exception of the neurons of the hippocampal region, which are formed to a large extent after birth, most of the neurons that populate the brain are generated in the fetus and, therefore, the prenatal period is the most critical for normal brain development.
The aim of this study was to establish whether it is possible to rescue the neurodevelopmental alterations that characterize the trisomic brain with a prenatal pharmacotherapy with Fuoxetine, a drug that is able to restore post-natal hippocampal neurogenesis in the Ts65Dn mouse model of Down’s syndrome.
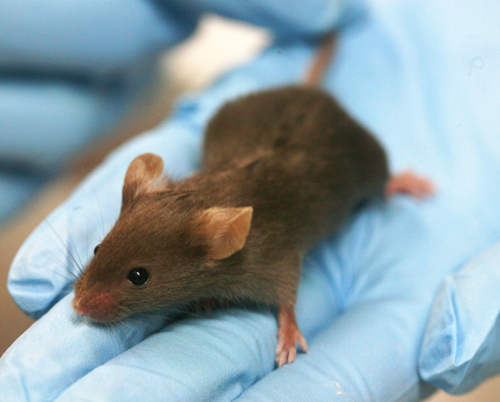
| A Ts65Dn mouse model of Down’s Syndrome |
The procedure of the experiment was to treat pregnant Ts65Dn females with fluoxetine from embryonic day 10 until delivery.
On post-natal Day 2 the pups received an injection of 5-bromo-2-deoxyuridine and were sacrificed after either 2 h or after 43 days (at the age of 45 days).
Untreated 2-day-old Ts65Dn mice exhibited a severe neurogenesis reduction and hypocellularity throughout the forebrain (subventricular zone, subgranular zone, neocortex, striatum, thalamus and hypothalamus), midbrain (mesencephalon) and hindbrain (cerebellum and pons).
In embryonically treated 2-day-old Ts65Dn mice, precursor proliferation and cellularity were fully restored throughout all brain regions.
The recovery of proliferation potency and cellularity was still present in treated Ts65Dn 45-day-old mice.
Moreover, embryonic treatment restored dendritic development cortical and hippocampal synapse development and brain volume.
The cognitive deficits caused by Down's syndrome have long been considered irreversible.
Importantly, these effects were accompanied by recovery of behavioural performance.
The current study provides evidence that a pharmacotherapy with fluoxetine during embryonic development is able to fully rescue the abnormal brain development and behavioural deficits that are typical of Down’s syndrome.
If the positive effects of Fluoxetine on the brain of a mouse model are replicated in human foetuses with Down’s syndrome, Fluoxetine (a drug usable in humans) may represent a breakthrough for the therapy of intellectual disability in Down’s syndrome.
If the positive effects of Fluoxetine on the brain of a mouse model are replicated in human foetuses with Down’s syndrome, Fluoxetine (a drug usable in humans) may represent a breakthrough for the therapy of intellectual disability in Down’s syndrome.
At last, as observed by Renata Bartesaghi (team leader of this research) :"Only clinical trials will tell us, however, whether such drug therapy, so effective in this mouse model of Down syndrome can achieve the same positive results in humans".
Prenatal pharmacotherapy, rescues brain development in a Down’s syndrome mouse model, 2013
Down Syndrome: progress in the search for a potential prenatal care