DEPRESSION AMONG PATIENT WITH CKD
WHAT IS CHRONIC KIDNEY DISEASE?

Chronic kidney disease (CKD) involves a gradual and permanent loss of kidney function. The number of functioning nephrons can lead to a worsening of anaemia, the inability to remove water, the onset of arterial hypertension, hyperphosphatemia, hypocalcemia, metabolic and isosthenuric acidosis (permanently isotonic urine compared to plasma with the loss of concentration and dilution ability), sometimes combined with heart disease and pericarditis. From a functional point of view, CKD involves an analogous and measured deterioration of both kidney blood flow and glomerular filtration. Therefore the degree of function loss is usually determined on the basis of the glomerular filtration rate. Approximately 13% of the general adult population has signs of CKD and is categorised in one of the five stages set by the*National Kidney Foundation Disease Outcomes Quality Initiative*(K/DOQI ). Frequency rises to 15-30% among the elderly and is over 50% in patients affected by heart disease and metabolic disorders.
Treating CKD
The therapy for CKD is first and foremost diet or conservative management. Right from the earliest phases of kidney impairment, a reduction in protein and phosphate intake is advisable, though the risk of malnutrition caused by excessively limited protein intake should be avoided, as should an excessively low calorie intake, which often should actually be higher than the calorie intake recommended for people of the same age, gender and weight.
End-stage chronic kidney disease is treated with a substitute therapy which involves substituting kidney function, at least in part, with dialysis or a kidney transplant.
There are two types of dialysis: peritoneal dialysis or haemodialysis.
Peritoneal dialysis

Haemodialysis

http://aou.udine.it/formazione/elenco-tesi/il-vissuto-emotivo-del-paziente-in-emodialisi-studio-fenomenologico/il-vissuto-emotivo-del-paziente-in-emodialisi-studio-fenomenologico
http://www.shireitalia.it/shire-italia/nefrologia-insufficienza-renale.aspx
DEPRESSION
Major depressive disorder, or MDD, is a mental or Mood disorder which features episodes of depression generally accompanied by low self-esteem and a loss of interest or pleasure in activities that would normally be considered pleasant (anhedonia).
https://en.wikipedia.org/wiki/Mental_disorder
BIOLOGICAL CAUSES OF DEPRESSION
Depression is an illness caused by a number of factors, where genetic, psychological, environmental and domestic as well as biochemical factors all contribute to its onset.
Biologically speaking, the causes can be attributed to the following:
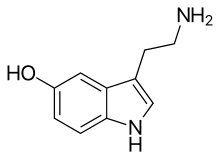
- Biogenic amines: the two neurotransmitters most involved in affecting mood disorders are noradrenaline and serotonin, whose levels are believed to be below-average in depressed people. The cause for this reduction in monoamines could be ascribed to an excessive lack of monoamine oxidase A, which metabolises monoamines.
- Neuroendocrine imbalance: several changes in neuroendocrine levels have been detected. The link between elevated cortisol and depression has now been generally accepted.
- Kindling: this is a physiological process where repeated stimulation of a particular area of the brain causes a seizure. In this case, kindling is believed to affect the temporal lobe.
- Genetic factors: it is estimated that 30-40% of depression is hereditary.
- Neuro-anatomical aspects: changes to the limbic system, basal ganglia, the hypothalamus as well as a reduction in size of the hippocampus.
Serotonin
Noradrenalin

CKD AND DEPRESSION
Depression among the elderly, particular those with chronic physical ailments, is a common problem, but also a complex one that is sometimes not easily identified, especially where there is a combination of somatic and mental symptoms.
A recent meta-analysis has estimated that the frequency of depression among patients with chronic kidney disease is 20%, whilst 23% of those on dialysis are depressed. It has also been proven that depression in CKD is linked to a worsening of a patient's clinical profile, with more frequent and longer hospital stays, a reduction in treatment"compliance":https://it.wikipedia.org/wiki/Compliance_(medicina) and higher death rates. Despite these circumstances, the rate at which depression is identified and treated among patients with chronic kidney disease remains low.
The use of drugs to treat depression among patients with CKD poses particular problems. In general, antidepressants bind to proteins and are then metabolised in the liver, but they are not removed to any significant degree with dialysis and this makes the removal of the metabolites of such drugs difficult to calculate. Further problems are posed by anticholinergic effects, including urinary retention from TCAs, the accumulation of toxic metabolites caused by SNRIs and an increased risk of bleeding from SSRIs. In any case, treatment using antidepressants in patients with CKD requires that drug dosage be adjusted according to the estimated glomerular filtration rate. To date, it is not yet clear if the treatment of depression in patients with CKD improves their kidney function.
http://www.progettoasco.it/numero-1-gennaio-2015-la-depressione-nei-pazienti-anziani-con-patologie-somatiche-quando-e-come-intervenire/#.VdYnlJco6f5
THE EFFECTS OF DEPRESSION ON CKD TREATMENT
Depression can indirectly affect a patient's outcome, influencing their nutritional state, their adherence to treatment and life expectancy. A lack of appetite can affect the quantity and quality of foods eaten, thus resulting in a deterioration of a patient's nutritional state, which can have a detrimental effect on the disease. The symptoms of depression - such as a lack of motivation, a lack of concentration and apathy - can interfere with a patient's adherence to treatment. It has also been proven that the persistence of depression reduces life expectancy among patients undergoing haemodialysis; though it has not been proven to what degree the severity of depression influences life expectancy.
http://aou.udine.it/formazione/elenco-tesi/il-vissuto-emotivo-del-paziente-in-emodialisi-studio-fenomenologico/il-vissuto-emotivo-del-paziente-in-emodialisi-studio-fenomenologico
Conclusion
In conclusion, patients with CKD require continuous psychological support, not only to ensure their own physical and mental well-being, but also in order to improve the efficacy of treatment, whether it be dialysis, haemodialysis or a kidney transplant. In conquering their depression, patients can conquer the illness that caused it with the increase in self-esteem and the motivation to continue their treatment.