Tiziana Ruggiero (238561) & Francesca Bar (239273)
Several pain conditions localized to the craniofacial region show a remarkable sex-related difference in their prevalence.
● For example, temporomandibular disorders (TMD), a group of conditions that have, as their principal symptom, pain in the masticatory muscles and/or temporomandibular joints (TMJs) with palpation and during function (eg, chewing, mouth opening, speech) occur at a 50% higher rate in women than in men.
● Burning mouth syndrome, a condition characterized by intense burning pain usually from the tongue as well as occasionally the mucosal aspect of the lips and/or the anterior hard palate, occurs at a 90% higher rate in women than in men.
● Primary headache disorders also show significant sex-related differences in their incidence and prevalence.
● Tension-type headaches, which are often associated with a feeling of muscle strain or spasm in the neck/shoulder or temporalis muscles and are characterized by dull, aching, nonthrobbing pain that can be distributed unilaterally or bilaterally and referred to temporal, occipital, parietal, or frontal regions of the head occur at a 50% higher rate in women.
● Migraine headache, which is characterized by a severe pounding-throbbing head pain that is usually unilateral and referred to the temporal region, occurs at a 150-200% higher rate in women.
● In contrast, cluster headaches, severe, excruciatingly painful headaches that occur in groups, are 5 times more common in men than women.
Peripheral mechanism
As with TMDs and burning mouth syndrome, there is a fault of consistent pathophysiological change associated with primary headaches that make it difficult to definitively determine the underlying neurophysiologic mechanism for this type of pain. In all primary headaches, pain is perceived to come from within the cranium and thus current theories suggest that activation of neural pathways that transmit input from the dura play an important role in headache pain.
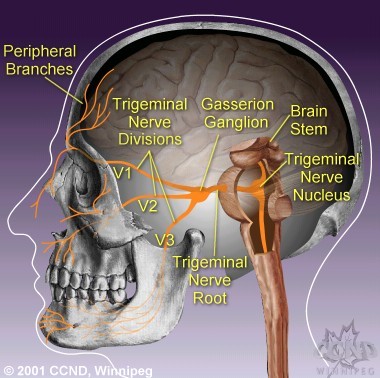
There is evidence for differences in afferent fibers that innervate craniofacial tissues associated with sex-related differences in pain, such as the masseter muscle and TMJ. One difference is that the expression of calcitonin gene-related peptide (CGRP), but not substance P or somatostatin, by trigeminal ganglion neurons that innervate the masseter muscle, is significantly higher in males than in females. While evidence to support an association between the release of CGRP by dural afferent fibers and the development of headache pain exist, there is no evidence for a direct excitatory or sensitizing effect of CGRP on dural afferent fibers.
Another sex-related difference in trigeminal afferent fiber response is seen when glutamate is used to excite Aδ and C fibers that innervate both the TMJ and masseter muscles. In this case, glutamate-evoked afferent discharge is significantly greater in females than in males.
Glutamate-evoked afferent discharge is mediated through activation of peripheral N-methyl-D-aspartate (NMDA) receptors in these tissues, and recent evidence suggests that sex-related differences in afferent response may be mediated through alterations in peripheral NMDA receptor function and/or expression.
A direct role for peripheral NMDA receptor mechanisms in the development of primary headaches has yet to be identified; however, cortical spreading depression, a central phenomenon thought to be associated with aura in migraine, appears to increase meningeal blood flow in part through peripheral NMDA receptor activation.
Central Mechanism
Virtually all trigeminal sensory neurons that respond to dural stimulation are reported to receive convergent cutaneous input from facial cutaneous receptive fields.
The high convergence of ophthalmic, cutaneous, and dural afferent fibers onto nociceptive trigeminal neurons may explain the referral of headache pain to the forehead and orbit region during migraine headache as well as the tender scalp which occurs during tension-type headache.
There is evidence for sex-related differences in the response properties of other trigeminal sensory neurons, such as those that respond to noxious stimulation of the TMJ. Inflammatory TMJ injury induces higher levels of the immediate early gene c-fos, an indicator of neuronal activation, in neurons in the caudal most part of the trigeminal sensory nucleus in female rats in proestrus (the estrous cycle stage associated with the highest levels of serum estrogen) than in male rats. Trigeminal sensory neurons that respond to noxious stimulation of the TMJ appear to have similar characteristics as those for dural activated trigeminal neurons, in particular a high degree of convergent cutaneous input from facial cutaneous receptive fields.
The greatest sex-related differences in the excitability of trigeminal neurons often occur during proestrus when serum estrogen levels are at their peak.
Estrogen receptors are found on trigeminal ganglion and sensory neurons, which indicates that both primary afferents and neurons are potential targets for estrogenic modulation of sensory input.
Estrogen replacement therapy in ovariectomized female rats increases the excitability of TMJ ganglion neurons recorded in vitro by decreasing activation threshold and causing the resting membrane potential to become more depolarized.
Gonadectomy significantly reduced glutamate-evoked jaw muscle reflex responses in females but not males, and estrogen treatment of gonadectomized females (and males) increased the magnitude of glutamate-evoked nociceptive jaw muscle reflex responses to a level similar to intact females. Taken together, these findings support the contention that sex-related differences in responses to noxious stimulation of the TMJ are due, at least in part, to estrogen-mediated alterations in the excitability of TMJ afferent fibers.
The response of afferent fibers after injection of glutamate into the masseter muscle and trigeminal sensory neurons after capsaicin application to the dura, is greater in proestrus than diestrus, which suggests that elevated levels of estrogen enhance the response of craniofacial fibers to certain noxious chemical stimuli. In contrast, the mechanical activation threshold of masseter muscle afferent fibers is positively correlated with plasma estrogen levels, which implies that as estrogen levels increase these fibers become less sensitive to noxious mechanical stimuli.
Relevance to human craniofacial pain
There is parallel evidence in humans suggesting at least some of the findings in animal models are also relevant to human craniofacial pain. In agreement with results in animals, injection of certain noxious chemicals (glutamate, capsaicin, serotonin) either under the skin of the face or into the masseter muscle evokes pain which is reported as more intense by women than men.
In healthy women and those suffering from TMDs there is some evidence that masseter muscle pressure pain soil, which reflect sensitivity to noxious mechanical stimuli, are lowest during the perimenstrual phase when estrogen levels are at their lowest.
This suggest that physiological mechanisms account, at least in part, for the increased prevalence of conditions such as TMD and migraine headache in women and the reported increase in TMD-related pains and migraine headache perimenstrually.
Reports
Headache as a side effect of combination estrogen-progestin oral contraceptives: A systematic review
The influence of gender and sex steroids on craniofacial nociception
The influence of estrogen on migraine: a systematic review