How does the system work
One of the most important molecules acting on hypothalamic arcuate nucleus is leptin, and it has been discovered that leptin receptors are also located in the ventral tegmental area (VTA) of the brainstem.
Leptin increase (an indication of enlargement of body fat stores) reduces firing of dopaminergic neurons, thereby decreasing food assumption, locomotor activity (and search for food) as well as sensitivity to highly palatable foods.
Leptin Receptor Signaling in Midbrain Dopamine Neurons Regulates Feeding. 2006
Moreover, it has been found out that insulin and glucose act on the mesolimbic pathway too: their boost has the same meaning, hence the same effects, of that of the leptin. However, whereas insulin operates on the VTA, as leptin, glucose influences the activity of neurons of the substantia nigra.
Adiposity signals and food reward: expanding the CNS roles of insulin and leptin. 2003
Glucose-regulated dopamine release from substantia nigra neurons. 2000
Besides, ghrelin too has a double action in appetite regulation: it acts both on the arcuate nucleus and ventromedial area of hypothalamus, and on the VTA. Ghrelin levels increase during fasting: it stimulates food intake and the pleasure sensation related to it.
In fact, if one has not eaten for several hours, one will spend more energies in seeking out food, and will experience a stronger gratification sensation from obtaining it.
Ghrelin induces feeding in the mesolimbic reward pathway between the ventral tegmental area and the nucleus accumbens. 2005

Highly palatable foods overwhelm the control mechanism
It seems all very logical so far. Thus where is the problem?
The point is that our organism has been evolving in an environment in which it was much more difficult to find food, and it still has not had enough time to adapt to the huge and rapid changes in its availability and caloric content that have been occurring during the last centuries.
Highly palatable foods (rich in sugars and lipids, and often visually attractive) stimulate reward pathways with such strength that their action prevails on the one of appetite-inhibiting substances: it often happens that, in spite of having had a large meal, we still find a place for dessert – which is normally the most caloric component of it.
Processed foods
Nowadays the trend is to largely produce highly processed foods, which are much more similar to drug in their action on the CNS: they strongly activate mesolimbic reward pathways, thence triggering the onset of addiction mechanisms.
In particular, foods with a high glycemic index (e.g. concentrated sugar) – foods containing carbohydrates that break down quickly during digestion and release glucose rapidly into the bloodstream – cause a rapid rise and fall in glycaemia after consumption, thus causing hunger after a few hours, and consequently leading to overeating.
Furthermore, processed foods are much easier to digest than non-processed ones, thus requesting lower energy consumption.
Food addiction: how processed food makes you eat more. 2013
Effects of dietary glycemic index on brain regions related to reward and craving in men. 2013
Fatty foods
Neural imaging studies have proved that the texture of fat in the mouth – this signal was once thought as the primary cue by which fats were perceived – is represented in areas of the cortex that have been implicated in chemosensory perception and sensory pleasure.
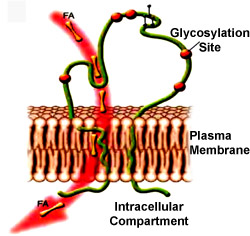
Moreover, in the last decade it has been demonstrated the existence of formerly-only-hypothesized fatty taste receptors: the long-chain fatty acid transporter CD36 and the G protein-coupled receptor GPR120. Variations in these genes might play a role in obesity; currently, however, we do not know if reduced fat sensitivity predisposes some individuals to obesity by promoting higher fat intake, or if chronic high-fat diet exposure leads to reduced fat sensitivity and obesity development.
 CD36
CD36
The taste for fat: new discoveries on the role of fat in sensory perception, metabolism, sensory pleasure, and beyond. 2012
CD36 may determine our desire for dietary fats. 2005
G protein–coupled receptors in human fat taste perception. 2011
The establishment of the addiction
How does our organism answer to this dysfunction of food intake control systems? By means of two mechanisms:
* Augmented release of leptin and insulin: the rise in their hematic concentrations goes together with body weight increase. However, they become progressively less effective, due to development of resistance phenomena.
Obesity and leptin resistance
- Down-regulation of D 2 R dopamine receptors in striatum: this neuroadaptive response can be observed in overweight subjects, and persists until body weight returns in normal range.
A rise in the activation threshold of reward circuits makes it necessary for overweight people to increase the assumption of highly caloric foods, in order to get the same gratification. This leads to the onset of compulsive-like eating.
Addiction-like reward dysfunction and compulsive eating in obese rats: Role for dopamine D2 receptors. 2010
The same behaviour is shown by subjects who display a particular polymorphism in D 2 R gene: TaqlAA1 allele.
Relation between Obesity and Blunted Striatal Response to Food is Moderated by TaqlA1 Gene. 2008
Vice versa, in food-restriction an increased sensibility of striatal neurons can be observed.
The same down-regulation of D 2 R phenomenon occurs in drug abuse and chronic alcoholism, and in fact people show compulsive-like drug- (or alcohol)-taking behaviour.
The discovery that obesity and drug addiction can be generated by the same neuroadaptive mechanisms confirms experimentally obtained data: it has been demonstrated that normally fed rats stop eating even the most delicious food when they expect a painful shock will occur, whereas rats fed with high-calorie foods keep feeding despite they know they will be hurt.
The same behaviour has been noticed in rats that were given unlimited access to cocaine or heroin.
Similarly, obese people know that eating high-calorie foods is dangerous for their health, and still they find extremely difficult to avoid them.
The fact that food addiction is possible, and that it is very similar to drug addiction, is furtherly proven by the finding that rats experimentally overfed with high-calorie foods experience the symptoms of withdrawal when they are treated with opioid antagonists (and consequently eat less).
Fatty foods may cause cocaine-like addiction. 2010
Nevertheless, while for drug and nicotine addiction it has been possible to identify a specific substance causing dependence, a similar factor has (still) not been detected in food addiction: it seems that this is triggered by the combination of sugars and lipids in high-calorie foods.
New pharmaceutical hypothesis
Finding out the analogy between drug and food addiction suggested that similar drugs could be used in their treatment. This led to commercialization of Belviq and Rimonabant, employed to reduce appetite in overweight or obese patients.
While the first one operates on serotonin receptor 5-HT 2C, the latter acts as an inverse agonist for the cannabinoid receptor CB 1 (also reducing smoke desire in smokers).
However, Rimonabant has been withdrawn from the market in Europe – and never approved in the USA – because it causes depression and suicidal ideation.
Nonetheless, this subject requires more study in the next years, and maybe it will lead to the discovery of new useful therapeutic strategies for obesity and related diseases, which are major death causes in developed Countries.