CHILDBIRTH
Childbirth or parturition is the expulsion of one or more newborn infants from a woman's uterus, at the end of a pregnancy. It consists of three stages: the shortening and dilation of cervix, the fetal expulsion and the birth of placenta.
- THE SHORTENING AND DILATION OF CERVIX
It’s divided in 2 phases. The first one is the latent phase or prodromal labor during which uterine contractions becomes regular and occur cervical dilation and effacement (thinning and stretching of the cervix). The active phase instead is characterized by three to four contractions every ten minutes, ropture of membranes, cervical dilation of 3 to 4 cm.
- THE FETAL EXPULSION
It begins when the cervix is fully dilated (10 cm) and so baby’s head can descent into pelvis up to the vaginal orifice. Now, the woman feels a pelvic pressure and a need of pushing. After the “crowning” (appearance of the fetal head at the vaginal orifice), the expulsion of the baby is complete and this stage ends.
- DELIVERY OF PLACENTA
This happens after its separation from the wall of the uterus and may require medical assistance.
There is also a fourth stage that’s called postnatal period or postpartum period or puerperio: it lasts about 6 weeks from childbirth.
All these stages are regulated by hormones which play a very important role. Some example of these hormones are:
- Oxytocin – it causes uterus’ contractions
- Progesterone – it is produced by placenta during pregnancy; when its level decreases, childbirth starts
- Catecholamines – they prepare the body for labour
- Endorphins – they reduce pain
- Estrogens – they increase uterus’ sensibility to oxytocin
- Relaxin – it changes collagen in pubic shymphysis relaxing it
PAIN AND ITS CONTROL
Pain is an unpleasant feeling signaling a tissue damage. It includes nociception, that is the nervous activity, and subjective experience or psychic state of pain.
NOCICEPTION : It is defined as "the neural processes of encoding and processing noxious stimuli". It is the afferent activity produced in the peripheral and central nervous systems by stimuli that have the potential to damage tissue.
First of all, there are peripheric nociceptors, sensitive to mechanical, thermal and chemical stimuli. By C and Aδ fibers these stimuli reach root ganglia and so the spinal cord in dorsal horn where central extensions of neurons of root ganglia enter into synapsis with secondary sensitive neurons. These stimuli then go up along the spinal cord in neospinothalamic tract (lateral, for C fibers) and paleospinothalamic tract (medial, for Aδ fibers) arriving finally in the thalamus. The thalamus projects with the lateral system to the somatosensory cortex in order to discriminate pain and with the medial system to other areas, important for affective and emotional component of pain.
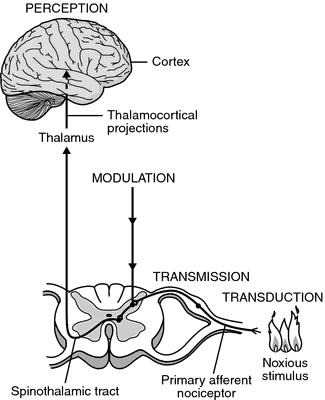
PAIN CONTROL : exist two mechanisms that allow pain control and create the endogenous analgesia system.
- Gate control theory – It is an ascending inhibitory system where collateral branches of Aβ fibers (stimulated by mechanical stimuli) excite inhibitory interneurons that inhibit synapsis between neurons of root ganglia and spinal sensitive neurons. In this way, the gate is closed and pain transmission locked. This mechanism is used in TENS(09)00572-0/abstract in order to reduce pain: TENS is transcutaneous electric nerve stimulation that stimulates Aβ fibers.

- Descending inhibitory system – If some areas (such as prefrontal cortex, parietal cortex, orbitofrontal cortex, anterior cingulate cortex, hypothalamus, thalamus, amygdala) are stimulated, we have “analgesia induced by stimulation”. These areas project on the periaqueductal grey matter and the nucleus raphes magnus that, via dorsolateral funiculus, send informations in spinal dorsal horns. They finally inhibit secondary sensitive neurons in spinal cord.
This descending inhibition happens in stress or dangerous situations or for psychological, social and cultural factors. It uses different neurotransmitters like opioids (endorphins, enkephalines, dynorphins), endocannabinoids or serotonin.

PAIN IN CHILDBIRTH
The pain of childbirth has 2 particularities: it’s intermittent with some pauses because of endorphins and it’s caused by a physiological (not pathological) event. Pain of childbirth is due to stretching of muscular fibers of cervix and uterus’ contractions in the first stage; in the second stage it’s created by stretching and lacerations of vagina, perineum and vulva.
- RESPONSE OF BODY : during childbirth, there are 2 main hormones that reduce pain.
- OXYTOCIN - It is a mammalian neurohypophysial hormone (secreted by the posterior pituitary gland) that acts primarily as a neuromodulator in the brain. Oxytocin plays an important role in the neuroanatomy of intimacy, specifically in sexual reproduction, in particular during and after childbirth. It is released in large amounts after distension of the cervix and uterus during labor, facilitating birth, maternal bonding, and, after stimulation of the nipples, lactation. Both childbirth and milk ejection result from positive feedback mechanisms.
Oxytocin is a peptide of nine amino acids (a nonapeptide).
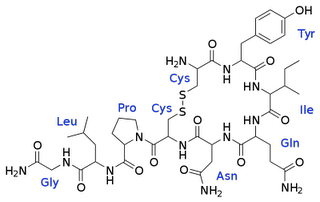
Oxytocin receptors are expressed by the myoepithelial cells of the mammary gland and in both the myometrium and endometrium of the uterus at the end of pregnancy. They are also present in the central nervous system where modulate a variety of behaviors. The oxytocin receptor belongs to the G-protein coupled receptor family, specifically Gq : this means its activity is mediated by G proteins that activate several different second messenger systems. Probably, oxytocin’s mechanism acts through calcium signaling (released by sarcoplasmic reticulum) that activates a protein kinase C; this kinase phosphorylates and so activates kinases of light chain of myosin. So, finally, we have contraction of smooth muscle.

Oxytocin has peripheral and central actions. Peripheral actions are the letdown reflex (important in breastfeeding), modulation of inflammation, sexual arousal, antidiuretic action, modulation of hypothalamic-pituitary-adrenal activity and uterine contraction. Central actions on the other hands are social behavior, maternal behavior, romantic attachment and preparing fetal neurons for delivery.
LETDOWN REFLEX : suckling by the baby at the nipple stimulates release of oxytocin that make contract mioephitelial cells of mammal gland.

UTERINE CONTRACTION : estrogens increase number of oxytocin receptors on the uterus, so when oxytocin is released by pituitary gland during birth, the uterus is very sensitivity to oxytocin. It causes contraction of smooth muscle and in this way makes the descent of baby possible. There is a positive feedback between release of oxytocin and cervical dilation: uterine contractions induced by oxytocin push the baby towards cervix and so it is stretched, this stretching stimulate new release of oxytocin.
MATERNAL BEHAVIOR : oxytocin is involved in the initiation of maternal behavior, not in its maintenance.
PREPARING FETAL NEURONS FOR DELIVERY : oxytocin silences fetal brain and so reduce its vulnerability to hypoxia.
PAIN CONTROL DURING CHILDBIRTH : oxytocin plays an important role in the modulation of pain. It acts on periaqueductal grey matter and it has been proved that an intra-PAG injection of oxytocin increases the pain threshold, whereas local administration of OXT receptor antagonist decreases the pain threshold. An experiment evidences this: the concentrations of OXT, endorphins and enkephalins in the PAG perfusion liquid of the rat increase after the pain stimulation; the concentrations of endorphins and enkephalins in the PAG perfusion liquid are decreased by the OXT receptor antagonist; the increased pain threshold induced by the OXT is attenuated by naloxone, an opiate receptor antagonist and the concentrations of endorphins and enkephalins in the PAG perfusion liquid are increased by exogenous OXT administration. This is because OXT, increasing intracellular concentration of calcium, could regulate the production of mediators, like endocannabinoids that are able to suppress pain pathways; however only central administration of OXT shows a significant antihyperalgesic activity.
In conclusion we can say that oxytocin has an analgesic effect.
- ENDORPHINS – they are endogenous opioid peptides that function as neurotransmitters. They are produced by the pituitary gland and the hypothalamus in vertebrates during exercise, excitement, pain, spicy food consumption, love and sexual activity and they resemble the opiates in their abilities to produce analgesia and a feeling of well-being. The name “endorphin” consists of “endo-” and “-orphin” that mean “endogenous” and “morphine” because endorphins produced by own body are hormones with morphine-like action.
The most important endorphin of our body is β-endorphin. It is a peptide, 31 amino acids long, resulting from processing of the precursor proopiomelanocortin (POMC) and it is released into blood from the pituitary gland and into the spinal cord and brain from hypothalamic neurons; it has behavioural effects.

Endorphins act on opioid receptors (opioids are endorphins, dynorphins, enkephalins and others) that are a group of G protein-coupled receptors with opioids as ligands. They are distributed widely in the brain. There are four major subtypes of opioid receptors: δ, κ, μ and nociceptin receptor; β-endorphin binds µ receptor which is called μ because its main ligand is morphine.
These receptors through a G-protein inhibit adenylate-cyclase, facilitate opening of potassium channels and inhibit also opening of calcium channels; in this way they cause hyperpolarization and inhibition of transmitter's release and so an inhibition of the synaptic transmission of pain.
Because of this, endogenous activation of opioid receptors provides relief from acute pain; however, the mechanisms of long-term opioid inhibition of pathological pain have remained hard to comprehend.
Opioid receptors are involved in problems related to opioid tolerance: this happens due to loss of connection between receptor and G protein and internalization of receptor. In the first case, with an experiment on male Wistar rats, it is proved a significant decrease in the mRNA and protein levels of Gαi and Gβ in the lumbar spinal cord of trained rats, responsible for exercise-induced morphine insensitivity. In the second case, because of the phosphorylation on receptor’s intracellular loops and consequent internalization of the receptor , there is a lower response to opioid; so protein kinase C activation (and consequent phosphorylation) plays an important role in morphine-induced μ-opioid receptor desensitization and tolerance development.
Endorphins have many actions, first of all control of pain.
RUNNER’S HIGH : this effect can occur anytime that people engage in any strenuous exercise or activity and it consists in a endorphins’ release during exercise that mitigate pain sensation and cause feelings of euphoria.
DEPERSONALIZATION DISORDER : the opioid antagonists naloxone and naltrexone have both been proven to be successful in treating depersonalization.
RELAXATION
PAIN CONTROL DURING CHILDBIRTH : finally we can say the main effect of endorphins is the hypoalgesic effect. They are involved in the descending inhibitory system and so they lock pain transmission through nociceptive pathway in all conditions, also in childbirth and pregnancy.
There are many studies about this that prove the endorphins-induced increase pain threshold during pregnancy.
The first one studies pain threshold during pregnancy in rats: data show a gradual rise in the pain threshold between 16 and 4 days prior to parturition and a more abrupt rise 1 to 2 days before that event and they also demonstrate the activation during pregnancy of an endorphin system that is apparently quiescent in nonpregnant female rats.
Role of endorphins in pregnancy and also in parturition is shown in sow too: response times to a thermal stimulation rise from week 12 to 5 days before parturition and they continue to rise until the birth of the first piglet; then they fall over days 1, 2 and 7 post-partum. After administration of naloxone (antagonist of opioid receptor) response times fall compared to control animals. So these results suggest that nociceptive threshold increases during late pregnancy in the sow, perhaps as an endogenous defence against labour pain, and that during parturition this change in nociceptive threshold is opioid-mediated.
An other study underlines how endorphins-induced analgesia acts in human normal vaginal delivery and not in caesarian section: concentrations of β-endorphin in mothers delivered vaginally are significantly higher than those in mothers delivered by cesarean section; on the other hand, there is no difference in neonatal levels of β-endorphin. These findings indicate that neither the presence or absence of labor affects fetal plasma β-endorphin secretion but the stress of labor and delivery produces a marked increase in maternal release of β-endorphin.
We conclude that pregnancy and parturition are associated with significant changes in levels of endorphins and suggest that they mediate changes in pain perception and maternal behavior during pregnancy and parturition.
- PHARMACEUTICAL CONTROL Different measures for pain control have varying degrees of success and side effects to the woman and her baby.
- Nitrous oxide gas – It is inhaled and it must be prescribed in Europe, not in UK
- Pethidine ( first synthetic opioid) - It may be used early in labour, as well as other opioids such as fentanyl, but if given too close to birth there is a risk of respiratory depression in the infant.
- Regional anesthetics epidurals (EDA) – It is the most popular medical pain control and it is a generally safe and effective method of relieving pain in labour. Epidural anaesthesia is performed into the epidural space which is the space inside the bony spinal canal between dura mater and arachnoid mater with cerebrospinal fluid.

It’s good: for analgesia alone (without anaesthesia, like in childbirth); as an adjunct to general anaesthesia; as a sole technique for surgical anaesthesia; for post-operative analgesia, after an operation where the epidural technique was used as the sole anaesthetic or in combination with general anaesthesia; for the treatment of back pain; for the treatment of chronic pain or palliation of symptoms in terminal care.
It’s different from spinal anaesthesia because: epidural anaesthesia needs a larger dose of drug, the onset of analgesia is slower with epidural anaesthesia, an epidural injection may be performed anywhere along the vertebral column, it is easier to achieve segmental anaesthesia using the epidural route, an indwelling catheter is more commonly placed in the setting of epidural anaesthesia.
IN CHILDBIRTH it is more effective than nitrous oxide, opioids, TENS and other common modalities of analgesia. So it gives a better pain relief, but it is associated with longer labour, more operative intervention (particularly instrument delivery) and increases in cost. Furthermore, pain, fear and stress hormones decrease upon administration of epidural analgesia, but may rise again later.
COMPARISON BETWEEN NON PHARMACEUTICAL AND PHARMACEUTICAL CONTROL
Pharmaceutical control causes more risks and complications postpartum; for example, it acts on the function of urinary bladder. A study(10)00176-1/abstract shows that the median times for sensation to return to the bladder in patients who have had a vaginal delivery without epidural analgesia is less long than ones in women who have had vaginal delivery with epidural analgesia and cesarean delivery under spinal anesthesia. So, we can consider normal vaginal delivery better for normal body’s function after parturition.
On the other hand, with epidural anaesthesia, in addiction to have a significant reduction in pain, women have greater maternal satisfaction. This is demonstrated by a study performed with 70 pregnant women, 35 of whom have received CSE anesthesia while 35 have received only non-pharmacological forms of pain relief during labor. Evaluating visual analogue scale (VAS) pain score, maternal satisfaction, the patient's intention to request the same technique in a subsequent delivery and loss of control during delivery, we can say that the use of CSE is associated with a significant reduction in VAS pain scores during delivery and with greater maternal satisfaction.