DESCRIPTION
Ezetimibe is the first example of a new class of drugs which selectively inhibits cholesterol absorption mainly in small intestine.

A really useful association?
Ezetimibe/simvastatin
INDICATIONS
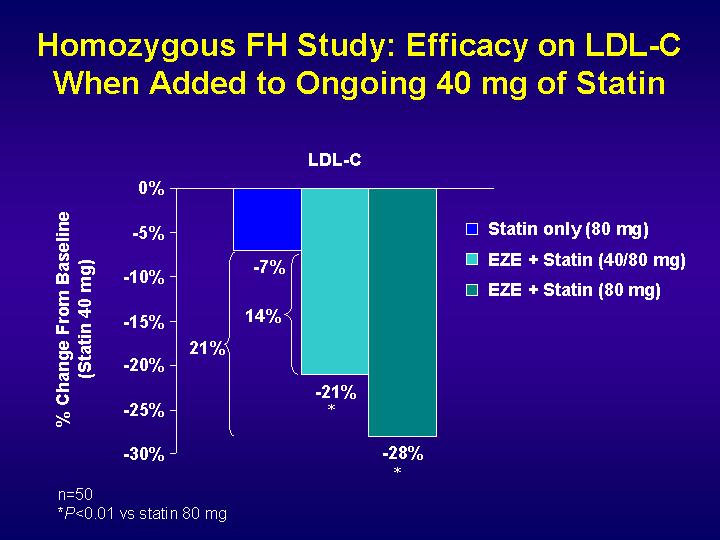
The administration of this new drug is indicated to lower plasmatic LDL cholesterol levels, in patients who cannot achieve cholesterol target levels with statins alone. The administration of a 10 mg dose each day, causes a 20% decrease in LDL cholesterol levels.
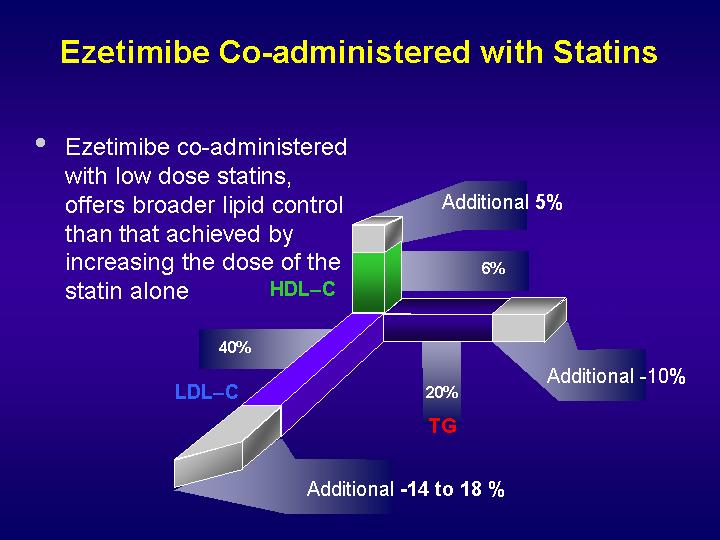
The action mechanism of the ezetimibe makes the co-administration with statins ideal. In fact, ezetimibe co-administered with statins can reduce LDL cholesterol levels up to 40%. This is an alternative way to reduce cholesterol levels, instead of increasing the dose of statins. In fact, because of the differences in the action mechanism between ezetimibe and statins (that reduce endogenous cholesterol synthesis, by inhibiting HMGCoA-Reductase, the key enzyme of this metabolic pathway), these two co-administered drugs work with a sinergic mechanism. Moreover, this approach allows many more patients to get the target cholesterol level.
MOLECULAR MECHANISM
Niemann-Pick C1–like 1 (NPC1L1) is a transmembrane protein involved in sterol transport through biological membranes, that seems to be the molecular target of ezetimibe.
p<>.This protein was originally identified on the apical membrane of enterocytes of mice and humans.
However, unlike mice, in which NPC1L1 is mainly expressed in the intestine, humans highly express NPC1L1 in the liver, localizing to the canalicular membrane of hepatocytes.
Since NPC1L1 allows the enterocyte to absorb natural cholesterol, in a recent study it was hypothesized that hepatic NPC1L1 allows the retention of bile cholesterol by hepatocytes and that ezetimibe disrupts hepatic function of NPC1L1.
To test this hypothesis, transgenic mice expressing human NPC1L1 in hepatocytes were created (while wild type mice do not express NPC1L1 in liver cells).
Hepatic overexpression of human NPC1L1 resulted in a 10- to 20-fold decrease in bile cholesterol concentration, but not phospholipid and bile acid concentrations. This decrease was associated with a 30%–60% increase in plasma cholesterol, mainly because of the accumulation of apoE-rich HDL. Bile and plasma cholesterol concentrations in these animals were virtually returned to normal with ezetimibe treatment. These findings suggest that also in humans, ezetimibe may reduce plasma cholesterol by inhibiting NPC1L1 function in both intestine and liver, and hepatic NPC1L1 may have evolved to protect the body from excessive loss of cholesterol through bile.
Hepatic Niemann-Pick C1–like 1 regulates bile cholesterol concentration and is a target of ezetimibe
About the mechanism of cholesterol transport from the canalicular bile into hepatocytes, many hypotesis were made:
1. As an apical transporter for cholesterol uptake, NPC1L1 could directly carry cholesterol from bile to hepatocyte cytoplasm;
2. NPC1L1 partitions cholesterol away from the pool that is normally delivered to ABCG5/ABCG8 for bile secretion;
3. NPC1L1 may interfere with the cholesterol transporting activity of ABCG5/ABCG8 without affecting ABCG5/ABCG8 protein levels.
p<>. In addition it was noticed that NPC1L1 colocalized with a canalicular ATP Binding Cassette, ABCB1 and this ATPase could play a role in NPC1L1 cholesterol transport.
SIDE EFFECTS
When administered in monotherapy, ezetimibe is generally well tolerated. The most important side effects are gallstone formation, because of increase in bile cholesterol secretion, so that the use of this drug in individuals predisposed to gallstone disease should be evaluated.
When co-administered with statins, side effects are the same as the administration of statins alone.
Ezetimibe/Simvastatin Side Effects
Endocrine side effects of HMG-CoA reductase inhibitors have included gynecomastia and thyroid function abnormalities.
TOXICITY
Ezetimibe does not seem to be metabolized by cytocrome p450 enzymes. Data show a low incidence of reduction in liver functionality when ezetimibe is co-administered with statins. Liver functionality exams should be asked before administering ezetimibe and then every two-four months.
The structure and function of Niemann-Pick C1-like 1 protein 2008
Purpose of review: Intestinal absorption and biliary excretion of cholesterol represent two major pathways by which the body regulates cholesterol homeostasis. Niemann-Pick C1-like 1 (NPC1L1) is a polytopic transmembrane protein containing a sterol-sensing domain of unknown function. In 2004, NPC1L1 was identified to be essential for intestinal cholesterol absorption, a process that is sensitive to a cholesterol absorption inhibitor ezetimibe. This review summarizes recent studies on NPC1L1 function and proposes a model for NPC1L1-dependent cholesterol uptake.
Recent findings: Cell culture experiments have shown that NPC1L1 mediates cellular uptake of various sterols but seems to have lower affinity to plant sterols than cholesterol. Transgenic animal studies have demonstrated that hepatic NPC1L1 has the potential to regulate biliary cholesterol excretion. Cholesterol and many transcriptional factors appear to regulate NPC1L1 gene expression. NPC1L1 protein is enriched in the apical membrane of polarized cells and its intracellular itineraries are clearly regulated by cholesterol availability. Evidence suggests cholesterol-regulated clathrin-mediated endocytosis is likely the cellular basis for NPC1L1-dependent cholesterol uptake, which may reconcile disagreement regarding NPC1L1 subcellular localization.
Summary: NPC1L1 may have evolved at two sites (apical membrane of enterocytes and canalicular membrane of hepatocytes) to mediate cholesterol uptake through a clathrin-mediated endocytic process, protecting the body against fecal and biliary loss of cholesterol.
Aggiunta di ezetimibe a statina riduce Ldl ossidate
Giungono dal Libano, e più esattamente dalla Divisione di Cardiologia dell'Università Saint-Joseh di Beirut, chiarimenti sugli effetti additivi apportati da ezetimibe alla riduzione della colesterolemia-Ldl quando cosomministrata alle statine. Rabih R. Azar, primo ricercatore, e il suo team hanno focalizzato l'attenzione sulle modifiche determinate da ezetimibe sulle Ldl ossidate (ox-Ldl), essendo queste ultime un elemento predittivo di eventi cardiovascolari avversi più affidabile rispetto ai consueti parametri lipidici. Un totale di 100 pazienti con malattia coronarica o equivalente sono stati randomizzati a ricevere un trattamento con atorvastatina 40 mg/die ed ezetimibe 10 mg/die oppure atorvastatina 40 mg/die e placebo. Sono state effettuate misurazioni di colesterolo-Ldl, sottofrazioni di colesterolo-Ldl e ox-Ldl al basale e dopo otto settimane di terapia. Il gruppo ezetimibe ha fatto registrare una maggiore diminuzione di colesterolemia-Ldl totale rispetto al placebo. Ciò è apparso dovuto principalmente a una più evidente riduzione (24% vs 10%, p=0,008) delle particelle grandi e flottanti di Ldl-c (large buoyant Ldl cholesterol). I livelli di ox-Ldl non sono cambiati nel gruppo placebo (50 /- 13 vs 51 /- 13 U/L) mentre sono diminuiti in quello ezetimibe, da 51 /- 13 a 46 /- 10 UI/L. La modificazione nel valore di ox-Ldl è risultato correlato in modo significativo con quello delle Ldl totali e delle "large buoyant" Ldl, ma non con quello delle Ldl piccole e dense, delle Hdl o delle Vldl. In conclusione, secondo gli autori, questo studio dimostra che ezetimibe fa diminuire il colesterolo ossidato attraverso il calo della colesterolemia-Ldl totale e delle particelle grandi e flottanti di Ldl-c.
Am J Cardiol, 2010; 106(2):193-7
Effect of ezetimibe/atorvastatin combination on oxidized low density lipoprotein cholesterol in patients with coronary artery disease or coronary artery disease equivalent. 2010
NPC1L1 localization
Inactivation of NPC1L1 causes multiple lipid transport defects and protects against diet-induced hypercholesterolemia, 2005