The Wolff Chaikoff effect: a biochemical way of prevention after accidental radioactive iodine exposure
Marco Fantini, Giovanni Cattaneo

INTRODUCTION
One of the major risks in case of a nuclear reactor accident consists in the emission and diffusion of radio-iodines (mainly I-131) in the atmonsphere. As a consequence, radioactive-ions may be inhaled or ingested thus accumulating in the thyroid, causing relevant irradiation and significant increase of thyroid cancer risk.
Iodide isotopes are greatly produced during fission reactions in nuclear reactors. These isotopes, with other radionuclides, may only be released and dispersed in the environment when the reactor core is damaged and the outer containments breached. Today, nearly all nuclear power plants in Western Europe and US are equipped with multiple containment structures and multiple core cooling systems. However, worldwide, many reactors which lack modern safety standards are still operating and a significant number of accidents are regularly reported. The most severe accident of the last decades was the Chernobyl disaster, on April 1986. Besides, the most recent nuclear accident was the Fukushima’s one, which occurred on March 2011.
Ingestion of potassium iodide (KI) determines the block of thyroid iodine uptake and inhibition of thyrocyte activity. This biochemical phenomenon is called Wolff Chaikoff effect, whose knowledge and application can protect against irradiation after accidental exposure to radioactive iodine.
Metabolism and kinetics of iodine

Iodine is a rare essential element whose sources are, for example, sea food, milk and iodized salt; its dietary requirements are 100-200 μg/die in the adults. Iodine is absorbed in the digestive tract as iodide (I-) and mainly cleared by kidney. Renal iodine clearance is not influenced by the uptake (not adaptive and not saturable). Once in the bloodstream, iodide uptake from thyroid is mediated by the NIS (Na/I symporter) a plasma membrane glycoprotein localized in the baso-lateral membrane of thyrocytes. Ioidide is then translocated into the follicular lumen (the colloid) by Pendrin (PDS). Iodide is finally organified on the tyrosyl residues of Tg in a TPO-catalysed reaction, in the presence of H 2 O 2, which is produced by
DOUX.
The Wolff Chaikoff effect

The Wolff Chaikoff effect is an inhibition of thyroid function in the presence of plasma iodide excess. In physiological condition, this phenomenon guarantees regular thyroid hormone secretion in response of variable dietary iodine levels. Various experiments revealed that an excess of intracellular iodide (≥10-3 M) inhibits several metabolic processes such as:
• Iodide organification: Braverman and Ingbar showed that high iodide concentrations inhibited organification in vitro. (CHANGES IN THYROIDAL FUNCTION DURING ADAPTATION TO LARGE DOSES OF IODIDE.1963)
Morand et al found that iodide causes an inhibition of NADPH oxidase activity and a reduction of H 2 O 2 release. Northern blot studies showed reduction in TPO mRNA levels. (Effect of iodide on nicotinamide adenine dinucleotide phosphate oxidase activity and Duox2 protein expression in isolated porcine thyroid follicles.2003)
• Hormone secretion: Becks et al found an inhibitory effect of elevated iodide concentration on thyroid hormone secretion while Corvilain et al showed that, while TSH enhance secretion through activation of cAMP pathway, iodide has an inhibitory role. (Regulation of differentiated thyroid function by iodide: preferential inhibitory effect of excess iodide on thyroid hormone secretion in sheep thyroid cell cultures. 1987) (Role of the cyclic adenosine 3',5'-monophosphate and the phosphatidylinositol-Ca2+ cascades in mediating the effects of thyrotropin and iodide on hormone synthesis and secretion in human thyroid slices. 1994)
• Iodide uptake: Braverman and Ingbar showed lower uptake activity in adapted thyroid after high iodide exposure in vitro. (CHANGES IN THYROIDAL FUNCTION DURING ADAPTATION TO LARGE DOSES OF IODIDE.1963)
Despite extensive investigations, the molecular basis of the biochemical modifications occurring in Wolff Chaikoff effect are not clearly understood yet. However, researchers have attempted to identify molecules involved in the thyroid regulation by iodide. Iodinated lipids seems to have a central role as mediators of the biochemical inhibiting pathways in thyroid. The most studied compounds probably involved in the iodide-mediated inhibition are:
• Iodolactones: Boeynaems and Hubbardshowed that arachidonic acid can be converted into a iodolactone (6-iodo- 8,11,14-eicosatrienoic-delta-lactone) in rat thyroids. (Transformation of arachidonic acid into an iodolactone by the rat thyroid.1980) Chazenbalk and collaborators synthesized an iodoarachidonate derivative and observed an iodide uptake inhibition with concentrations as low as 10(-8) M The authors also reported an inhibition of organification with higher concentrations (10(-5) M) of this iodocompound. (In vitro inhibitory effects of an iodinated derivative of arachidonic acid on calf thyroid.1984) Dugrillon et al suggested a physiological role of iodolactone in inhibiting thyroid growth by reducing EGF-induced proliferation. (Evidence that an iodolactone mediates the inhibitory effect of iodide on thyroid cell proliferation but not on adenosine 3',5'-monophosphate formation.1990)
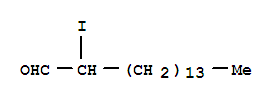
• 2-iodohexadecanal (2-IHDA): as suggested by Pereira et al, the biosynthesis of this compound is likely to involve the addition of iodine to the vinyl ether group of plasmalogens. (Identification of a major iodolipid from the horse thyroid gland as 2-iodohexadecanal.1990) It was then observed that 2-IHDA inhibited in vitro both NADPH oxidase and TPO (Inhibition of thyroid NADPH-oxidase by 2-iodohexadecanal in a cell-free system.1994) and that this effect may be due to PLC pathway inhibition (Inhibition of H2O2 production by iodoaldehydes in cultured dog thyroid cells.1994). Panneels et al also showed that 2-IHDA inhibits AC activity (which is instead stimulated by TSH).(Inhibition of human thyroid adenylyl cyclase by 2-iodoaldehydes.1994)
Recently, Leoni et al confirmed with PCR analysis that iodide excess inhibits the expression of essential genes for thyroid acitvity: TSHr, NIS, Tg, and TPO. (Differential gene expression analysis of iodide-treated rat thyroid follicular cell line PCCl3.2008)
Escape from wolff chaikoff effect
The Wolff Chaikoff effect lasts for about 2 days and is followed by an escape phenomenon, which is associated with a decrease in thyroid NIS mRNA and NIS protein, as observed by Eng et al. (Escape from the acute Wolff-Chaikoff effect is associated with a decrease in thyroid sodium/iodide symporter messenger ribonucleic acid and protein.1999) As a consequence, a decrease in iodide transport into the thyroid takes place, lowering the intrathyroidal iodine content below a critical inhibitory threshold and allowing organification of iodide to resume. Juan C Solis-S et al recently showed that in case of iodide excess an inhibitory effect on thyroid iodotyrosine dehalogenase (tDh) and the iodothyronine deiodinase type 1 (ID1) takes place, thus reducing intrathyroidal dealogenation and contributing to the escape phenomenon by reduction of iodine recycling mechanism. (Inhibition of intrathyroidal dehalogenation by iodide.2011)

Counter-measures in case of radioiodine contamination
In case of a nuclear accident, radio-iodines may be released into the atmosphere and enter the exposed people’s bodies mainly through inhalation. In order to prevent thyroidal radioactive- iodide accumulation many strategies can be pursued: apart from remaining indoors, food restriction, evacuation, also Wolff Chaikoff effect has a key role in blocking thyroid, thus preventing from radioactive-ions accumulation and reducing radiation. This effect can be achieved by oral administration of KI, which is absorbed from the gastrointestinal tract in about 30-60 min. As showed by Verger et al, ingestion of 100 mg of iodide just before exposure to radioactive iodine blocks at least 95% of the thyroid dose. If exposure persists, daily administration of a 15 mg dose of KI would then maintain the thyroid blockade at a 90% level. However, to be effective, KI has to be taken shortly before or immediately after exposure. (Iodine kinetics and effectiveness of stable iodine prophylaxis after intake of radioactive iodine: a review.2001)
• Pregnant women, foetus and newborn: iodine crosses the placentar barrier and the foetus thyroidal uptake begins at 10-12 weeks but remain low until 22 weeks. From that moment on, it increases until term. Iodine also concentrates in maternal milk. Until 12th week, iodide prophylaxis is useless for the foetus, but harmless and useful for mother irradiation prevention. The most important foetal risk to prevent is neonatal iodine-induced hypothyroidism.
• Children and adolescents: benefits of KI prophylaxis are higher in these categories, as risk of radiation-induced thyroidal cancer is greater.
• Eldery adults: risk of KI side effects increases with age, unlike the benefits of KI, which are far less clear for the eldery than for children.
Side effects of KI prophylaxis
The possible adverse effects of KI prophylaxis are:
• Iodine-induced hyperthyroidism (IIH): has been observed after treatments with iodine-containing drugs (amiodarone) for long periods and after iodine prophylaxis in regions with iodine deficiency. This effect especially appears in people with poor dietary iodine uptake or, more frequently, in Grave’s disease or toxic multi-nodular goiters.
• Iodine induced hypothyroidism occurs when the escape from Wolff Chaikoff effect does not take place. This effect occurs more frequently in case of autoimmune thyroiditis, subacute thyroiditis or radioiodine treatment for thyrotoxicosis. Iodine-induced hypothyroidism is very frequent in newborns, especially in pre-term babies after a iodine overload of the mother either before delivery or during breast-feeding. This is due to low iodine levels and immaturity of iodine uptake regulation system in foetus. Undiagnosed, iodine-induced hypothyroidism may lead to long-term neurological and mental development (cretinism). Once diagnosed, hypothyroidism is easily treated by hormonal therapy.
• Non-thyroidal adverse effects: represented by allergic and anaphylactic responses to iodine. They may include fever, swelling, shortness of breath and rashes.
Sources:
From the molecular characterization of iodide transporters to the prevention of radioactive iodide exposure.2006
Iodine kinetics and effectiveness of stable iodine prophylaxis after intake of radioactive iodine: a review.2001