DEFINITION
The Lazarus phenomenon is described as delayed return of spontaneous circulation (ROSC) after cessation of cardiopulmonary resuscitation (CPR). This was first reported in the medical literature in 1982, and the term Lazarus phenomenon was first used by Bray in 1993.
PROPOSED MECHANISMS
The exact mechanism of delayed ROSC is unclear and it is possible that more than one mechanism is involved.
Positive end expiratory pressure
Rapid manual ventilation without adequate time for exhalation during CPR can lead to dynamic hyperinflation of lungs. Dynamic hyperinflation may lead to gas trapping and an increase in the end-expiratory pressure (called auto-PEEP) leading to delayed venous return, low cardiac output and even cardiac arrest in patients with obstructive airways disease. Auto-PEEP is a possible cause of pulseless electrical activity (PEA), and rapid ventilation during CPR should be avoided. Hypovolaemia and decreased myocardial contractility could exaggerate its effect on venous return and cardiac output. Some authors recommend discontinuing the ventilation transiently for 10 to 30 seconds in PEA to allow venous return.
Even though auto-PEEP due to dynamic hyperinflation seems most plausible and has some evidence in patients with obstructive airways disease, this alone would not explain all cases of delayed ROSC.
Ventilatory management of respiratory failure in asthma. 1993
Delayed action of drugs
It is possible that drugs injected through a peripheral vein are inadequately delivered centrally due to impaired venous return, and when venous return improves after stopping the dynamic hyperinflation, delivery of drugs could contribute to return of circulation. In general, cocaine is capable of inhibiting sodium, calcium and potassium channels. This capability, however, only applies to local anaesthetic doses that would never be achieved through general use, even during lengthy binges, and would rapidly lead to a fatal outcome. Under specific conditions, it is likely that similar concentrations may be achieved in localized areas, eliciting the onset of arrhythmias or epileptic convulsions (symptoms that may, alternatively, be induced by a vascular spasm accompanied by localized hypoxia). At doses markedly lower than those underlying the blockade of all channels, cocaine is also capable of interfering with calcium channel function (sensitive to calcium antagonists, including dihydropyridines , used in clinical contexts) and a specific potassium channel active in phase of repolarization of the action potential of cardiomyocytes. The myocardium is a target for these cocaine-elicited effects. L-type calcium channels present on the surface membrane of cardiomyocytes open during the rapid depolarization phase of the action potential (phase 0), so facilitating the slow influx of calcium that characterizes phase 2 (plateau) and are gradually inactivated, proceeding to the relaxation phase 3. The probability that these channels will open during the depolarization phase depends on their degree of phosphorylation, with phosphorylated channels being activated at a higher rate. Phosphorylation is mediated by the stimulation of cardiac ß-adrenergic receptors . Calcium influx inside the cardiomyocyte is fundamental in maintaining calcium concentration in the sarcoplasmic reticular system at the levels required by cardiac functions: sympathetic stimulation increases heart rate (as well as the rate of cycles of voltage-gated channel activation), phosphorylates the L-type channels and increases the intracellular calcium reserve. As a result, a greater quantity of calcium is released from the sarcoplasmic reticular system by the contractile apparatus, producing an increase in the contractile strength of the heart. Maintaining a balance between calcium influx, calcium output and the storage capacity of the sarcoplasmic reticular system is of the utmost importance: an excess of intracellular calcium may produce potentially fatal arrhythmias and elicit processes of cell deterioration resulting in apoptosis.
Cardiac complications including ischaemia and myocardial infarction have been reported both during cocaine intoxication and abstinence.
 cocaine
cocaine
In addition to cocaine effects on the heart also other drugs such as heroin which use includes scarred and collapsed veins, bacterial infections of the blood vessels and heart valves;
 heroin
heroin
methamphetamine cause a variety of cardiovascular problems, including rapid heart rate, irregular heartbeat, and blood pressure increased;
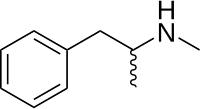 methamphetamine
methamphetamine
finally, doses of 10 mg of PCP or more cause dangerous changes in blood pressure, heart rate, and respiration, often accompanied by nausea, blurred vision, dizziness, and decreased of awareness of pain.
 PCP
PCP
Cardiovascular Complications of Cocaine Use,2009
Conseguenze mediche di abuso di droga
Hyperkalaemia
There are few reports of delayed ROSC in the presence of hyperkalaemia. It is a well-known fact that intracellular hyperkalaemia could persist longer, rendering the myocardium retractile for long periods of time.
Normal serum potassium levels are between 3.5 and 5.0 mEq / L , at least 95% of the body's potassium is found inside cells , with the remainder in the blood. This concentration gradient is maintained principally by the Na + / K + pump .The sodium potassium pump located on the membrane of cardiac cells extrudes sodium ions for potassium ions to enter, then thrown out of the three sodium ions sodium potassium pump, are then transformed into the heat exchanger, which takes advantage of energy gained to eliminate the cytoplasmic calcium. the coupled operation of these two pumps is neutral.
Under conditions where the sodium potassium pump does not work, or works poorly, it is to be affected the operation of the sodium-calcium exchanger, which means that if for some reason the sodium-calcium pump stops working, it stops working even exchanger sodium -calcium, and if it stops working latter, calcium accumulates in the cytoplasm; this is a mechanism at the base of a series of events, in particular, if the calcium accumulated in the cells can have cell death for cytotoxicity, then calcium accumulated becomes toxic.

Patient with hyperkalemia may develop clinical manifestations in many parts of the body including the gastrointestinal system, heart, kidney and neurological. A toxic effect most important of hyperkalemia are arrhythmias, but it can have an effect on peripheral muscles causing muscle weakness and respiratory paralysis ascending.
When potassium levels reach 6mEq /l may appear paresthesia, tachycardia and intestinal colic.
If the levels rise to 7mEq /l appear serious cardiac and neurological.
Increased extracellular potassium levels result in depolarization of the membrane potentials of cells. This depolarization opens some voltage-gated sodium channels , but not enough to generate an action potential. After a short while, the open sodium channels inactivate and become refractory , increasing the threshold needed to generate an action potential. This leads to the impairment of neuromuscular, cardiac , and gastrointestinal organ systems. Of most concern is the impairment of cardiac conduction which can result in ventricular fibrillation or asystole .
With mild to moderate hyperkalemia, there is reduction of the size of the P wave and development of peaked T waves . In severe hyperkalemia ECG complex can evolve to a sinusoidal shape. There Appears to be a direct effect of elevated potassium on some of the potassium channels that increases their activity and speeds membrane repolarization. The faster repolarization of the cardiac action potential causes the tenting of the T waves, and the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves.

sintomi nelle alterazioni elettrolitiche.
hyperkaliemia.
Transient asystole
It is possible that asystole after countershock could be transient before a perfusable rhythm restores circulation. Transient asystole following defibrillation would explain at least one case, where CPR was interrupted after a last cardioversion attempt resulting in asystole, and ROSC occurred soon after. However, transient asystole would not explain delayed ROSC in majority of patients in whom the duration of asystole was much longer. In another case, CPR was stopped while the patient was still in ventricular fibrillation and haemodynamic activity returned few moments later.
CELLS SURVIVAL AFTER DEATH
A new mechanism has been discovered that finely adjusts the synthesis of certain proteins considered necessary for cell survival. The mechanism involves a new class of RNA which, although not coding for any protein, is able to increase the cellular synthesis of specific proteins .These RNAs activity, defined antisense (AS), depends on their peculiar structure and by their ability to bind in a selective manner the mRNA coding for a specific protein.
When in the cell an RNA AS meets its mRNA, the synthesis of the protein encoded by the latter is increased.
This mechanism has been tested in cellular and animal models and it is believed that under certain conditions of stress, such as those induced by nutrient deficiency, it is important to promote cell survival. the cell responds to stress, a situation that can damage DNA, launching two action plans: one for checking the integrity of its genome (DNA) and to assess the possibility of survived the stressful situation, the other aimed an energy saving that is implemented via the decrease of cellular activities, including protein synthesis overall. In this system without further expenditure of energy - the production of sense and antisense RNA do not increase - is ensured the synthesis of proteins necessary for the transient cell survival.
Oxygen and glucose deprivation has almost immediate effects on brain function, typically causing symptoms in approximately 5–7 seconds. This dysfunction is also reflected in the electroencephalogram (EEG), generally consisting of an increase in slow wave activity and finally in the cessation of activity. These phenomena are a direct consequence of synaptic failure of pyramidal cells,reflecting the high metabolic demand of synaptic transmission.Recent findings in rats,showed disappearance of the EEG signal after approximately 15–20 s. Afterhalf a minute of electrocerebral silence, however, a slow wave with a duration of approximately 5–15 seconds appeared . It was suggested that this wave might reflect the synchronous death ofbrain neurons and was therefore named the ‘‘Wave of Death’’.

As regards the stem cells new researches has suggested that stem cells could actually survive in up to 2-day-old cadavers, but researchers had thought that dead bodies would be poor homes for any cells, lacking the oxygen and nutrients the body's cells need to stay alive. Apparently the stem cells were able survive in the total absence of oxygen in fact some of them have been found to functioning in cadavers after 14 days of death.
These stem cells in both dead mice and human corpses were dormant when discovered, with extraordinarily reduced metabolic activity, marking the first time scientists have found that stem cells were capable of such dormancy. The researchers suspect that chemicals given off after death , or the low levels of oxygen or nutrients in corpses, or a combination of all these factors, could have sent the stem cells into dormancy, helping them survive for weeks
neural Dynamics during Anoxia and the ‘‘Wave of Death’’.2011
CONSEQUENCES OF DELAYED RETURN OF SPONTANEOUS CIRCULATION
Delayed ROSC can lead to serious professional and legal consequences. Questions will be asked about whether CPR has been conducted properly and whether it was stopped too soon. The medical team might be accused of negligence and incompetence and even be sued for damages if a patient survives with severe disability. A doctor involved in resuscitation and certification of death followed by delayed ROSC has recently been accused of culpable homicide.
HOW WOULD ONE RECOGNIZE DEATH?
It is important to realize that death is not an event, but a process. The conference of Medical Royal Colleges in the UK advocated that death is a process during which various organs supporting the continuation of life fail. The physical findings to support this—absence of heartbeat and respiration—are the traditional and the most widely used criteria to certify death. Since these findings alone are not a sign of definitive death, it is quite possible to declare death in the interval between cessation of CPR and delayed ROSC.
Because delayed ROSC occurred within 10 minutes in most cases, many authors recommend that patients should be passively monitored for at least 10 minutes following unsuccessful CPR. During that period the family should be informed that CPR had been stopped because of poor response and further efforts are not in the best interests of the patient. It should also be mentioned that the patient is being closely monitored to establish death beyond any doubt. Death should not be certified in any patient immediately after stopping CPR, and one should wait at least 10 minutes, if not longer, to verify and confirm death beyond doubt.
Diagnosis of death. Memorandum issued by the honorary secretary of the Conference of Medical Royal Colleges and their Faculties in the United Kingdom on 15 January 1979.
Brain death.1978