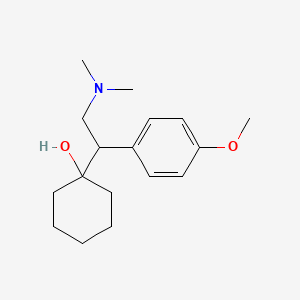
Description
Venlafaxine is an antidepressan of the serotonin- norepinephrine reuptake inhibitor (SNRI) class. First introduced by Wyeth in 1993, it is licensed for the treatment of major depressive disorder (MDD), as a treatment for generalized anxiety disorder, and comorbid indications in certain anxiety disorders with depression.
At low doses (<150mg/day), it acts only on serotonergic transmission.
At moderate doses (>150mg/day), it acts on serotonergic and noradrenergic systems, whereas at high doses (>300mg/day), it also affects dopaminergic neurotransmission.
Many doctors are starting to prescribe venlafaxine "off label" for the treatment of diabetic neuropathy (in a similar manner to duloxetine) and migraine prophylaxis (in some people, however, venlafaxine can exacerbate or cause migraines).
Studies have shown venlafaxine's effectiveness for these conditions. It has also been found to reduce the severity of 'hot flashes' in menopausal women and men on hormonal therapy for the treatment of prostate cancer.
Mechanism of action
Venlafaxine is usually categorized as a serotonin-norepinephrine reuptake inhibitor (SNRI), but it has been referred to as a serotonin-norepinephrine-dopamine reuptake inhibitor (SNDRI). It works by blocking the transporter "reuptake" proteins for key neurotransmitters affecting mood, thereby leaving more active neurotransmitters in the synapse. The neurotransmitters affected are serotonin and norepinephrine. Additionally, in high doses it weakly inhibits the reuptake of dopamine, with recent evidence showing that the norepinephrine transporter also transports some dopamine as well, since dopamine is inactivated by norepinephrine reuptake in the frontal cortex. The frontal cortex largely lacks dopamine transporters; therefore, venlafaxine can increase dopamine neurotransmission in this part of the brain.
Pharmacokinetics
Venlafaxine is well absorbed, with at least 92% of an oral dose being absorbed into systemic circulation. It is extensively metabolized in the liver via the CYP2D6 isoenzyme to desvenlafaxine (O-desmethylvenlafaxine), which is just as potent a SNRI as the parent compound, meaning that the differences in metabolism between extensive and poor metabolisers are not clinically important in terms of efficacy. Side effects, however, are reported to be more severe in CYP2D6 poor metabolisers. Steady-state concentrations of venlafaxine and its metabolite are attained in the blood within 3 days. Therapeutic effects are usually achieved within 3 to 4 weeks. No accumulation of venlafaxine has been observed during chronic administration in healthy subjects. The primary route of excretion of venlafaxine and its metabolites is via the kidneys. The half-life of venlafaxine is relatively short, so patients are directed to adhere to a strict medication routine, avoiding missing a dose. Even a single missed dose can result in withdrawal symptoms. Venlafaxine is a substrate of P-glycoprotein (P-gp), which pumps it out of the brain.
Dosage and administration
Venlafaxine should be administered in a single dose with food either in the morning or in the evening at approximately the same time each day. Each capsule should be swallowed whole with fluid and not divided, crushed, chewed, or placed in water, or it may be administered by carefully opening the capsule and sprinkling the entire contents on a spoonful of applesauce. This drug/food mixture should be swallowed immediately without chewing and followed with a glass of water to ensure complete swallowing of the pellets.
Major Depressive Disorder and Generalized Anxiety Disorder
For most patients, the recommended starting dose for Venlafaxine is 75 mg/day, administered in a single dose. For some patients, it may be desirable to start at 37.5 mg/day for 4 to 7 days, to allow new patients to adjust to the medication before increasing to 75 mg/day. Patients not responding to the initial 75 mg/day dose may benefit from dose increases to a maximum of approximately 225 mg/day. Dose increases should be in increments of up to 75 mg/day, as needed, and should be made at intervals of not less than 4 days, since steady state plasma levels of venlafaxine and its major metabolites are achieved in most patients by day 4.
Panic Disorder
It is recommended that initial single doses of 37.5 mg/day of Venlafaxine be used for 7 days. In clinical trials establishing the efficacy of Venlafaxine in outpatients with panic disorder, initial doses of 37.5 mg/day for 7 days were followed by doses of 75 mg/day and subsequent weekly dose increases of 75 mg/day to a maximum dose of 225 mg/day.
Side effects
Venlafaxine have a numerous side effects, but the principal is that, in some cases, may worsen depression and even cause suicidal thoughts.
Venlafaxine is not used in bipolar disorder because it can induce mania or mixed episodes.
It can be divided into:
Very common (>10% incidence):
Headache (tipically of most SSRI and that most often occurs at the beginning of therapy or after a dose escalation)
Nausea (tipically of most SSRI, and it is usually transient and less severe in those receiving the extended release formulations)
Insomnia
Asthenia
Dizziness
Ejaculation disorder (sexual side effects can be seen with virtually any antidepressant, especially those that inhibit the reuptake of serotonin)
Dry mouth
Common (1–10% incidence):
Constipation
Nervousness
Hypertension
Impotence
Tremor
Weight loss
Abnormal dreams
Serum cholesterol increased (when treatment is prolonged and it may be dose-dependent)
Uncommon (0.1-1% incidence):
Neck rigidity
Pelvic pain
Suicide attempt
Hypotension
Syncope
Tachycardia
Mucous membrane bleeding
Gastrointestinal bleeding
Abnormal liver function tests
Rare (0.01–0.1% incidence):
Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
Thrombocytopenia
Mania
Serotonin syndrome
Very rare (<0.01% incidence):
Anaphylaxis
QT prolungation
Delirium
Increasing of the eye pressure
Suicide

The US Food and Drug Administration body (FDA) requires all antidepressants, including venlafaxine, to carry a black box warning with a generic warning about a possible suicide risk.
A 2014 meta analysis of 21 clinical trials of venlafaxine for the treatment of depression in adults found that compared to placebo, venlafaxine reduced the risk of suicidal thoughts and behavior.
A study conducted in Finland followed more than 15,000 patients for 3.4 years.
Venlafaxine increased suicide risk 1.6- fold (statistically significant), as compared to no treatment. In another study, the data on more than 200,000 cases were obtained from the UK general practice research database. At baseline, patients prescribed venlafaxine had a greater number of risk factors for suicide (such as prior suicide attempts) than patients treated with other anti-depressants.
The patients taking venlafaxine had significantly higher risk of completed suicide than the ones on fluoxetine or citalopram. After adjusting for known risk factors, venlafaxine was associated with an increased risk of suicide relative to fluoxetine and dothiepin that was not statistically significant. A statistically significant greater risk for attempted suicide remained after adjustment, but the authors concluded that it could be due to residual confounding. An analysis of clinical trials by the FDA statisticians showed the incidence of suicidal behaviour among the adults on venlafaxine to be not significantly different from fluoxetine or placebo. Venlafaxine is contraindicated in children, adolescents and young adults. According to the FDA analysis of clinical trials venlafaxine caused a statistically significant 5-fold increase in suicidal ideation and behaviour in persons younger than 25. In another analysis, venlafaxine was no better than placebo among children (7–11 years old), but improved depression in adolescents (12–17 years old).
Contraindications
Studies of venlafaxine in paediatric age groups have not established its efficacy. Venlafaxine is not recommended in patients hypersensitive to it, nor should it be taken by anyone who is allergic to the inactive ingredients, which include gelatin, cellulose, ethylcellulose, iron oxide, titanium dioxide and hypromellose. It should not be used in conjunction with a monoamine oxidase
inhibitor (MAOI), as it can cause potentially fatal serotonin syndrome. Venlafaxine can increase eye pressure, so those with glaucoma may require more frequent eye checks. There are few well-controlled studies of venlafaxine in pregnant women. A study released in May 2010 by the Canadian Medical Association Journal suggests use of venlafaxine doubles the risk of miscarriage. Consequently, venlafaxine should only be used during pregnancy if clearly needed. Prospective studies have not shown any statistically significant congenital malformations. There have, however, been some reports of self-limiting effects on newborn infants. As with other serotonin reuptake inhibitors (SRIs), these effects are generally short-lived, lasting only 3 to 5 days,and rarely resulting in severe complications.
Drug interactions
Venlafaxine should be taken with caution when using St John's wort. (a medical herb).Venlafaxine may lower the seizure threshold, and coadministration with other drugs that lower the seizure threshold such as bupropion and tramadol should be done with caution and at low doses.
Experimental notes
Between december 2012 and december 2013, a team of researchers attempted to use Venlafaxine to relieve painful diabetic peripheral neuropathy. This study showed the efficacy of venlafaxine in pain reduction in patients with diabetic neuropathy .
In this study they used also pregabalin and carbamazepine.
Bibliography
http://www.rxlist.com/effexor-xr-drug/indications-dosage.html
http://www.ncbi.nlm.nih.gov/pubmed/24167687
http://en.wikipedia.org/wiki/Venlafaxine
http://chemistry.about.com/od/factsstructures/ig/Chemical-Structures---V/Venlafaxine.htm