Author: Paolo Mammucci
Definition
Neurogenic bladder is a term applied to a malfunctioning urinary bladder caused by neurologic dysfunction or insult due to internal or external trauma, disease or injury. It can develop as a result of a lesion at any level in the nervous system, including the cerebral cortex, spinal cord or peripheral nervous system. However the term “ neurogenic bladder” proves to be inappropriate, because it focuses attention on just one organ, the bladder, while actually it affects several organs, from kidneys to urethra. For the low urinary apparatus, firstly affected, the term neurogenic urethral-bladder dysfunction should be preferred. In fact, downline of bladder, there is the urethra, a very complex structure with lots of bundles, muscles and nerves and connected to the pelvic floor.

Neuroanatomy
The bladder is a balloon-shaped organ that serves as a kind of storage unit for urine. It is held in place by pelvic muscles in the lower part of the belly. Within the urethral-bladder apparatus, there are three different functioning areas: the detrusor muscle, the bladder neck (also called "smooth muscle") and the striated external sphincter.

Normal voiding is essentially a spinal reflex, modulated by the central nervous system (brain and spinal cord) which coordinates the functions of the bladder and urethra. The detrusor muscle is mostly innervated by parasympathetic fibers and it has a few adrenergic receptors. Although it is a smooth muscle, the detrusor is the only voluntary controlled smooth muscle! The bladder neck is mostly innervated by sympathetic fibers. The striated external sphincter is under voluntary control and receive innervation from pudendal nerve of somatic nervous system. During the course of a day, an average person will void approximately 4-8 times. The urinary bladder is in storage mode for most of the day, allowing an individual to engage in more important activities than urination. Normal bladder function consists of 2 phases—filling and emptying. The normal micturition cycle requires that the urinary bladder and the urethral sphincter work together as a coordinated unit to store and empty urine.
( Neurogenic Bladder physiology, Medscape, 2014 )
Pathophysiology and symptoms of the neurogenic bladder
In normal conditions, these three different “organs” have to work in coordination and synergy for guarantee an adequate storage and complete evacuation of urine. In healthy bladders, the change in bladder-filling pressure between empty and full is normally less than 10–15 cm H2O. Normal voiding pressures for males and females are from 50 to 80 cm H2O and from 40 to 65 cm H2O, respectively ( Pathophysiology of the neurogenic bladder, Pubmed, 2007). In patients with neurogenic urethral-bladder dysfunction, disordered innervation of the detrusor musculature and external sphincter adversely affects bladder function.

Functional alteration during collection phase leads to:
- Daytime/nighttime pollakiuria
- Detrusor Overactivity
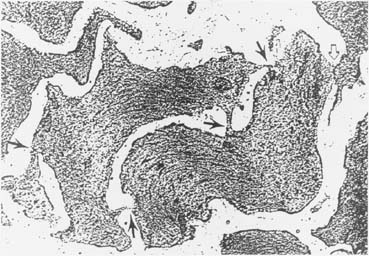
Dysjunction pattern in detrusor overactivity. Protrusion junctions are indicated (arrows). (From Elbadwi A: Structural basis of voiding dysjunction. In Ray S (ed): Female Urology, 2nd edn. Philadelphia, WB Saunders, 1995)
Functional alteration during voiding phase leads to:
- Bladder sphincter dyssynergia (or detrusor sphinter dyssynergia, or DSD)
Management of the neurogenic bladder
The therapy of all these pathologies depends on the physiopathological overview of the problem. The cornerstone of optimal “neurogenic urethral-bladder dysfunction” management is early identification and characterization (typology) and the institution of proactive therapy. Crucial for long-term prognosis of patients with NBSD is the fact that the management must start before consequences of bladder dysfunction become apparent. From the outset, the goals of management are to prevent or minimize secondary damage to the upper urinary tracts and bladder from the primary neurogenic bladder dysfunction and to achieve safe social continence. ( General principles and treatments goals, Pubmed, 2007 )
Diagnostic procedures
Usually doctor may order several tests of the nervous system and the bladder to diagnose neurogenic bladder:
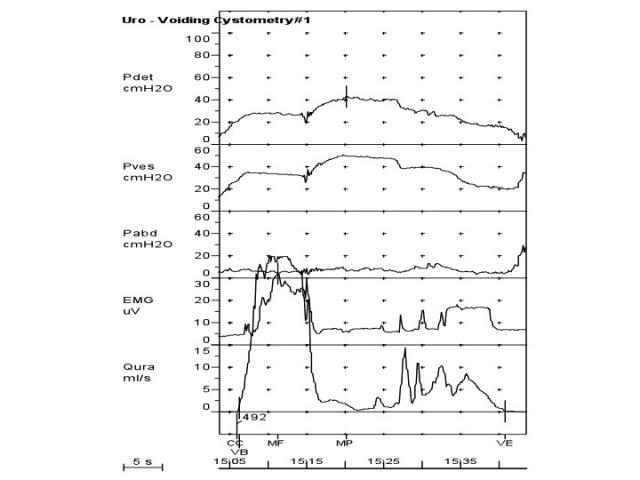
- Urodynamic studies (bladder function tests) are conducted to measure bladder capacity, bladder pressures, the flow of urine and bladder emptying. A cystoscopy may be performed to examine the inside of the bladder and urethra with a small telescope (cystoscope).

- The skull, spine, and urinary tract may be examined with X-rays, computed tomography (CT), and magnetic resonance imaging (MRI).

- Postvoid residual urine: it’s a part of basic evaluation. If the PVR is high, the bladder may be contractile or obstructed
- Cystogram: it helps to confirm the presence of stress incontinence, the level of urethral motion and the presence of a fistula or bladder diverticulum may be noted

Pharmacologic Treatment
There are three main categories of drugs used to treat urge incontinence including anticholinergic drugs, antispasmodics and tricyclic antidepressant agents.
1 Anticholinergic drugs : they are mostly used in women with urge incontinence because their effect is to inhibit involuntary bladder contractions. They can be also used in treating urinary incontinence associated with urinary frequency, urgency and nocturnal enuresis.The most common used anticholinergic drugs are:

1.1 Oxybutynin , the most commonly-used.Oxybutynin is a tertiary amine with a well-documented therapeutic effect on detrusor hyperactivity and its effectiveness is attributed to a combination of anticholinergic (+M3-selective receptor subtype antagonism+) and antispasmodic activity. In fact it has spasmolytic effects on bladder smooth muscle as a calcium antagonist and also works as a local anesthetic. "Several studies have shown its efficacy for decreasing the filling pressure, increasing the capacity of the neurogenic bladder and preserving renal function . The usual dose regimen of oral oxybutynin is 0.3–0.6 mg/kg per day in three doses" ( Pubmed, Pharmacologic treatment, 2007: anticholinergics ). Oxybutynin is also a possible treatment of hyperhidrosis.

1.2 Propantheline bromide is an antimusarinic drug used for hyperhidrosis, bladder spasms and involuntary urination ( enuresis ). It blocks the acetylcholine action at postganglionic parasympathetic receptor sites.

1.3 Hyoscyamine sulfate inhibits specifically the actions of acetylcholine on structures innervated by postganglionic cholinergic nerves and on smooth muscles that respond to acetylcholine but lack cholinergic innervation.

2 Antispasmodics drugs : their most important function is to relax the smooth muscles of the urinary bladder. They increase bladder capacity and effectively decrease or eliminate urge incontinence:
2.1 Tolterodine L-tartrate is a competitive muscarinic receptor antagonist; it decreases bladder contractions. Tolterodine acts on M2 and M3 subtypes of muscarinic receptors whereas older antimuscarinic treatments for overactive bladder act more specifically on M3 receptors. It has fewer side effects than oxybutynin.

2.2 Darifenacin works by blocking the M3 muscarinic acetylcholine receptor, which is primarily responsible for bladder muscle contractions.
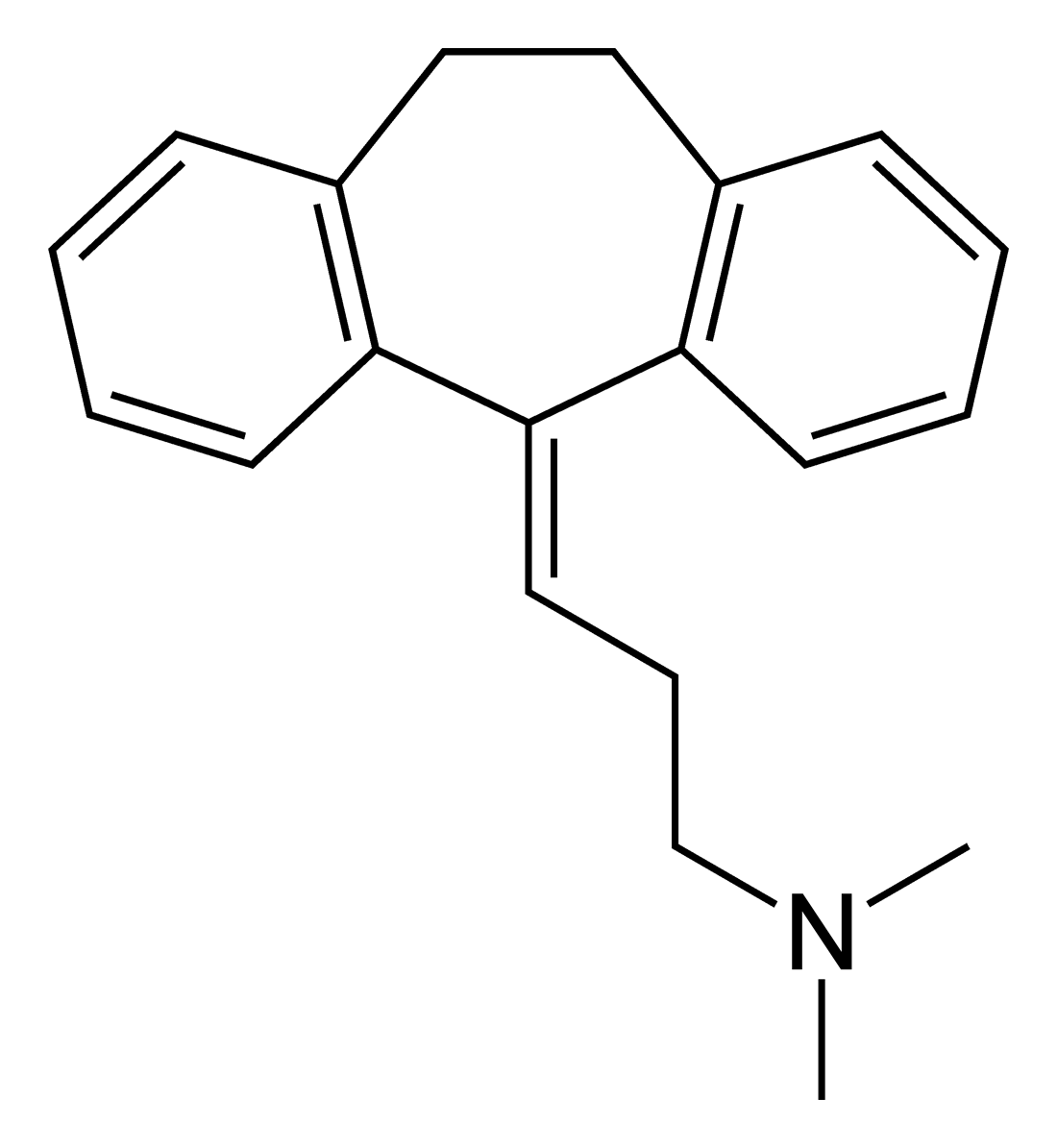
3 Tricyclic antidepressant agents: these kinds of drugs were historically used to treat major depression; however, they are also used for treating bladder dysfunction .These drugs classically act centrally and peripherally to block uptake of serotonin and norepinephrine. Furthermore, they appear to have anticholinergic and direct muscle relaxant effects on the urinary bladder. This mix of effects makes them useful in patient with overactive bladder and incontinence.
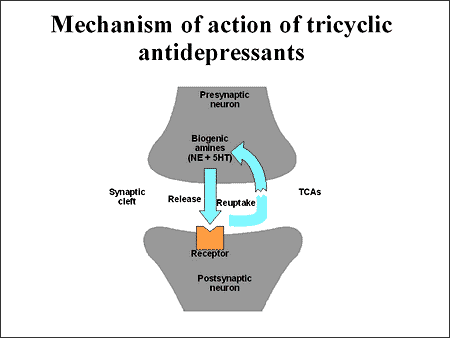
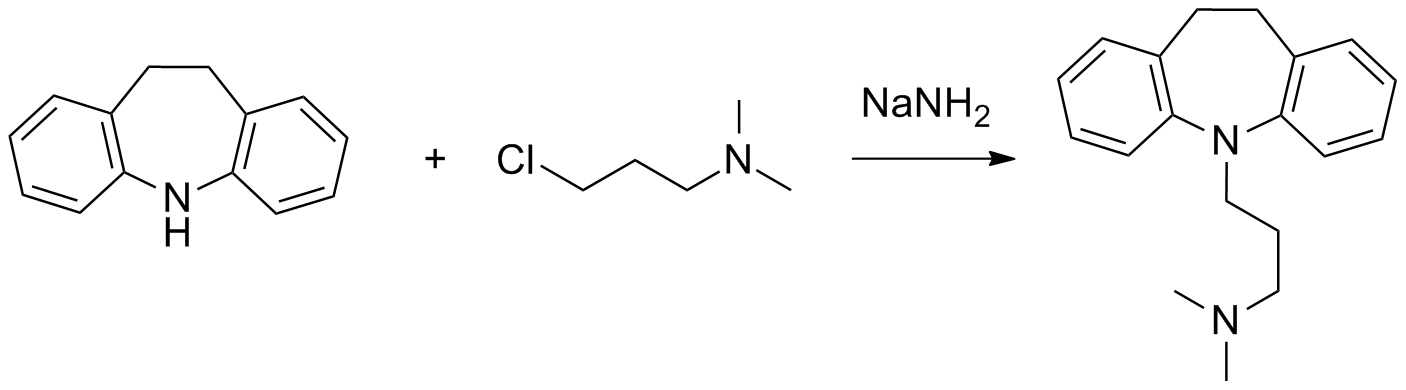
3.1 Imipramine : it’s the most used drug, for a long time used to treat primary nocturnal enuresis because of its ability to shorten the time of delta wave stage sleep, where wetting occurs. In addition, it facilitates urine storage by decreasing bladder contractility and increasing outlet resistance. It has alpha-adrenergic effect on the bladder neck and antispasmodic effect on detrusor muscle. Imipramine hydrochloride has a local anesthetic effect on bladder mucosa.
3.2 Amitryptiline hydrochloride : in addition to its antidepressant and sedative properties, it is extremely effective in decreasing symptoms of urinary frequency in women with pelvic floor muscle dysfunction. Amitriptyline hydrochloride restores serotonin levels and helps break the cycle of pelvic floor muscle spasms. It is well-tolerated and effective in most women with urinary frequency. However it is ineffective for use in urge incontinence.
Conclusions
Medical management with anticholinergic drugs is useful to provide safe urinary continence in more than 90% of patients with a neurogenic bladder. Early diagnosis avoids complications and allows an optimum management of bladder function with few side-effects on the neurogenic patient’s life.
" Therapeutic goals should no longer be restricted to prevention of secondary damage to both upper and lower urinary tracts. Instead, our goal should be to achieve normal renal and bladder growth at safe bladder pressure, with appliance-free continence." ( "The neurogenic bladder: medical treatment", Pubmed, 2007 )