Gian Maria Carlo Piutti
DEFINITION
Xeroderma pigmentosum (XP) is a rare autosomal recessive disease, characterized by hypersensitivity of the skin to ultraviolet (UV) radiation leading to high incidence of skin cancer and progressive neurological complications (acquired microcephaly, decreased or absent deep tendon reflexes, progressive sensorineural deafness, spasticity, ataxia, epilepsy and progressive cognitive impairment).
HISTORY
Xeroderma pigmentosum was described for the first time in 1870 in Vienna by Moritz Kaposi, a Hungarian professor of dermatology and in 1874 was named for the first time Xeroderma or parchment skin, while in 1882, the term 'pigmentosum' had been added to emphasize the striking anomaly of pigmentation.
EPIDEMIOLOGY
This disease involves both sexes and all races, with an incidence of 1:250.000 in the United States and a gene frequency of 1:200.
XP is roughly six times more common in Japanese people than in other groups.
The most common is the group C form.
ETIOPATHOGENESIS
The most common defect in xeroderma pigmentosum is an autosomal recessive genetic defect in which nucleotide excision repair (NER) enzymes are mutated. Ultraviolet (UV) light can causes pyrimidine dimers in DNA that have the potential to lead to mutations and cancer; these dimers are excise by NER enzymes.
Patients with XP are at a high risk for developing skin cancers, such as basal cell carcinoma
Specifically, exposure to UV light causes DNA damage. The absorption of high energy light leads to the formation of pyrimidine dimers, namely cyclobutane-pyrimidine dimers and pyrimidine-6-4-pyrimidone photoproducts.

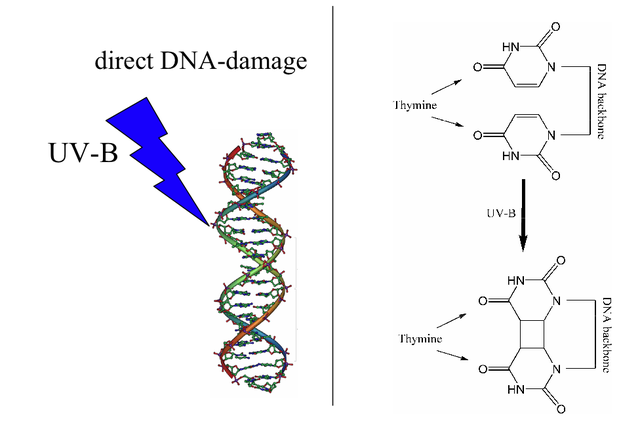
In humans the damage is first excised by endonucleases. DNA polymerase then repair the missing sequence, and ligase "seals" the transaction. This process is known as nucleotide excision repair.

TYPES
There are seven subgroups, plus one variant form:
| Type | Gene | Locus | Also know as/description |
|---|
| Type A, I, XPA | XPA | 9q22.3 | Xeroderma pigmentosum group A- the classical form |
| Type B, II, XPB | XPB | 2q21 | Xeroderma pigmentosum group B |
| Type C, III, XPC | XPC | 3p25 | Xeroderma pigmentosum group C or classic form |
| Type D, IV, XPD | XPD ERCC6 | 19q13.2-q13.3 , 10q11 | Xeroderma pigmentosum group D or De Sanctis-Cacchione syndrome |
| Type E, V, XPE | DDB2 | 11p12-p11 | Xeroderma pigmentosum group E |
| Type F, VI, XPF | ERCC4 | 16p13.3-p13.13 | Xeroderma pigmentosum group F |
| Type G, VII, XPG | RAD2 ERCC5 | 13q33 | Xeroderma pigmentosum group G |
| Type V, XPV | POLH | 6p21.1-p12 | Xeroderma pigmentosum variant |
- XPA is a protein of uncertain function, its role seems to be checking the correct position of other proteins in the context of DNA damage so that it could be affected by specific nucleases.
- XPB and XPD are subunits of the transcription factor TFIIH and have both helicase activity
- XPC recognizes the site where the DNA is damaged along with HR23B
- XPE is a subunit of a heterodimer that binds specifically to the damaged DNA and stimulates the etching reaction.
- XPF and XPG are nucleases
- XPV / POLH encoding DNA polymerase eta (Pol η)
SIGNS AND SYMPTOMS
Various clinical aspects and intensity of signs are described according to the gene involved (7 known complement groups) and type of mutation. In extreme cases, exposure to sunlight must be forbidden; as such, individuals with the disease are often colloquially referred to as Children of the Night .
The group A patients tend to develop neurological problems in early childhood, while those of group D in late childhood. The patients of group C instead do not develop problems of this type.
In group D showing children of short stature, brittle hair and low intelligence, in Group C will get ataxia.
Symptoms include:
- Skin signs:
- Severe sunburns when exposed to only small amounts of sunlight
- Development of many freckles at an early age
- Solar keratoses and skin cancers on the exposed areas (hands, arms, face)
- Telangiectasias
- Scaly skin
- Limited growth of hair on chest and legs
- Dry skin
- Irregular dark spots on the skin
- Ocular signs: photophobia, often the first sign, before cutaneous lesions; followed by bilateral cataract; increased risk of ocular benign and malign tumors
- Neurological signs (14 to 40% of patients): more severe central nervous system disorders are observed when mutations occur in XPA DNA binding site
- mental retardation, pyramidal syndrome, peripheral neuropathia

DIAGNOSIS
Physical examination and genetic counseling

- PRENATAL DIAGNOSIS:
- Amniocentesis
- Chorionic villus sampling
- Culture of amniotic cells
- POSTNATAL DIAGNOSIS:
- Culture of skin fibroblasts
- Skin biopsy
PROGNOSIS
The risk of developing skin cancers other than melanoma is 10.000 times higher than that observed in the general population, and risk of developing melanoma before age 20 is greater than 2.000.
Multiple basal cell carcinomas (basaliomas) and other skin malignancies frequently occur at a young age (often occurs before the child is 5 years old).
In fact, metastatic malignant melanoma and squamous cell carcinoma are the two most common causes of death in XP victims.
Less than 40% of individuals with the disease survive beyond the age of 20. Some XP victims with less severe cases do manage to live well into their 40s ( 2/3 die before adult age ).
The life expectancy increases in patients who avoid sunlight and who undergo regular follow-ups to assess and treat skin cancers.
The prognosis is good in patients without neurological disorders and scrupulously protect from UV rays.
TREATMENT
There is no cure for the XP, the most obvious, and often crucial part of treatment, is avoiding exposure to sunlight (even the light coming through windows and fluorescent bulbs is dangerous).
- sunscreens
- UV-proof clothing
- indoors protection with anti-UV films

Isotretinoin (also known as 13-cis retinoic acid) has been shown to reduce the incidence of epithelial tumors in patients with XP due to its role in the modulation of keratinocytes differentiation.
Vitamin D deficiency is common, which can be treated with supplements.
Keratoses can also be treated using cryotherapy or fluorouracil
FOLLOW-UP
- Regular check-ups of skin and eyes
- Treatment of cancerous lesions