GASTRINOMA
DEFINITION:
A gastrinoma is a tumor in the pancreas or duodenum that secretes excess of gastrin.
Gastrinomas are most commonly found in the duodenum (50-70%) and less commonly in the pancreas (20-40%): they occur as single tumors or as small, multiple tumors. About one-half to two-thirds of single gastrinomas are cancerous (malignant) tumors that often spread to the liver and nearby lymph nodes.
Non-beta-cell pancreatic gastrinomas may be associated with Zollinger-Ellison Syndrome (ZES), which is seen at low frequency in man. Furthermore, many patients with gastrinomas have several tumors as part of a condition called multiple endocrine neoplasia type I (MEN I). MEN I patients often have tumors of the pituitary gland and parathyroid glands, as well as tumors of the pancreas.
Gastrin physiological role
Under physiological conditions, Gastrin is synthesized in G cells, which are located in gastric pits, primarily in the antro-pyloric mucosa of the stomach, and binds receptors found predominantly on parietal and ECL cells. About 90% of GI gastrin is in the antral tissue and 10 % is in the duodenum. Gastrin is a major physiological regulator of gastric acid secretion and has also an important trophic or growth-promoting influence on the gastric mucosa.
Gastrin is a linear peptide that is synthesized as a preprohormone and is post-translationally cleaved
in three biologically active forms:
• G-14 (14 amino acids): mini gastrin;
• G-17 (17 amino acids): little gastrin;
• G-34 (34 amino acids): big gastrin.
The five C-terminal amino acids (pentagastrin) are identical to those in CCK, which explains their
overlapping biological effects. Pentagastrin is used to stimulate parietal cells during tests of gastric secretory function.
The active forms of gastrin, G-17, G-14 and G-34, are about equipotent in their ability to stimulate acid secretion and about 1500 times more potent, on a molar basis, than histamine, which also stimulates the parietal cell to secrete acid. G-17 is the principal secretion of the antrum. Its plasma concentration rises during the digestive phase, and it is believed to be the main physiologic form of the hormone that is released in response to a meal. Gastrin's circulatory half-life varies with molecular size but is of few minutes. Gastrin is metabolized by many tissues throughout the body.
The G cell is a classic gut endocrine cell with microvilli on the luminal surface that mediate the
detection of food within the stomach. Gastrin is released by explosive exocytosis, an activity modulated by endocrine, paracrine, neurocrine and local luminal factors. The primary stimulus forsecretion of gastrin is the presence of certain foodstuffs, especially peptides and certain amino acids (particularly phenylalanine and tryptophan) in the gastric lumen. Elevated calcium in serum or gastric lumen, alcoholic beverages, and coffee also are effective stimuli for gastrin release. Antral G cells are also stimulated to produce gastrin by vagus nerve stimulation (anticipation of a meal, sight, smell, and initial taste of food, gastric distension). Distension of the gastric walls acts reflexly to cause gastrin release: these reflexes operate through long, vago-vagal and short, enteric nervous system pathways. Cholinergic vagal fibers synapse on intrinsic nerve fibers containing gastrin-releasing peptide (GRP), also known as bombesin, which in turn innervate the antral G cell. GRP receptors activate the phosphoinositide pathway via a pertussis-toxin-insensitive G-protein, probably of the Gq/G11 class. Vagal stimulation leads to GRP release and gastrin secretion. Antral G cells are also stimulated to produce gastrin by increased gastric pH: the secretion of gastrin is inhibited when the lumenal pH of the stomach becomes very low. Gastrin release is partially inhibited at an antral luminal pH of 3.5 and completely inhibited at a luminal pH of 2.
Somatostatin (SS), which is secreted by D cells and acts as a paracrine agent, controls gastrin secretion by the G cell through modification of gastrin gene transcription. D cells are also present within the oxyntic mucosa and SS release can inhibit gastric acid secretion by local diffusion through the intercellular space or the local mucosal circulation. Thus, SS can inhibit acid production by both direct (parietal cell) and indirect mechanisms (decreased histamine release from enterochromaffin-like cells and decreased gastrin release from G cells). Vagal fibers also innervate, via the enteric nervous system, the antral D cells, which secrete SS. The
interneuron in this case is cholinergic and its effect on D cell secretion is inhibitory. GRP can also have a negative regulatory role in the fundic mucosa by directly mediating the release of SS by the D cell. Thus, vagal stimulation results in gastrin release and inhibition of SS secretion. The D cell, however, is directly stimulated by H+. As gastric acidity increases, SS secretion
increases and gastrin release is inhibited.
Gastrin release is also inhibited by secretin. Secretin is released from duodenal S cells in response to luminal acid and long-chain fatty acids.
Gastrin is released into the circulation from secretory granules along the baso-lateral border, in close proximity to mucosal blood vessels. Following exocytosis from the G cell, gastrin is transported to its site of action, the oxyntic mucosa of the stomach, in an endocrine manner.
Gastrin interacts with the CCK-B (or CCK2) receptor (CCK2R) on parietal cells and enterochromaffin-like (ECL) cells. In this way it stimulates acid secretion directly and potentiates the release of histamine, which in turn interacts with the parietal cell to induce further gastric acid secretion.

Nature Reviews Cancer 6, 936-946 (December 2006)
Gastrin appears to have at least two major effects on gastrointestinal function:
* Stimulation of gastric acid secretion.
Gastrin receptors are found on parietal cells and ECL
cells. The binding of gastrin, along with histamine and acetylcholine, leads to fully-stimulated acid secretion by those cells.
* Promotion of gastric mucosal growth.
Gastrin clearly has the ability to stimulate many aspects
of mucosal development and growth in the stomach. Treatment with gastrin stimulates DNA, RNA and protein synthesis in gastric mucosa and increases the number of parietal cells. In its absence,
gastric and intestinal mucosa will atrophy unless exogenous gastrin is administered. Gastrin is also a weak stimulant of pepsinogen secretion.
The gastrinoma cells are not subject to the same feedback regulations that control antral G-cell secretion of gastrin, and their gastric secretion is spontaneous and continual. Hypergastrinemia is associated with gastric hyperplasia and gastric acid hypersecretion, leading to ulceration in the stomach, duodenum, small intestine.
SYMPTOMS:
Gastrinoma causes the following symptoms:
▪ hypergastrinaemia;
▪ ulcers of the duodenum, stomach, and small intestine;
▪ diarrhea and steatorrhea;
▪ generalised cancer symptoms.
The persistent hypergastrinemia results in hypersecretion of gastric acid: this is due to both gastrin’s trophic effects, which increases the parietal cell mass, and the stimulatory effect of persistent high gastrin levels on oxyntic cell acid secretion.
Consequences include peptic ulcer, and the hypersecretion of HCl also causes hyperperistalsis and inhibits the activity of lipases, causing severe diarrhea, steathorrea and hypokalemia.
These effects are all related to the low pH in the intestinal lumen, caused by the large volumes of acidic gastric contents delivered to the small intestine. The ability of pancreatic and intestinal secretions to neutralize the gastric acid is overwhelmed. The large volume of secretion, impaired intestinal absorption, and increased motility associated with non-physiologically high gastrin levels all contribute to the diarrhea. The low intestinal luminal pH causes bile salts to precipitate and inactivates pancreatic lipase, resulting in failure to digest and absorb dietary fat, leading to its consequent appearance in the stool (steatorrhea). Most GI secretions are high in potassium and, when these are lost in diarrhea, hypokalemia may ensue.
DIAGNOSIS:
Diagnosis is based on the patients history which is typically characterized by recurrent episodes of peptic ulcer disease or by severe reflux esophagitis and/or diarrhea or by acid-related symptoms which fail to respond to standard treatment regimens. Upper gastrointestinal tract endoscopy will provide evidence for peptic ulcer disease in anatomical regions located aborally the duodenal bulb within the descending part of the duodenum or even farther distally within the jejunum. Peptic ulcers frequently occur in groups indicating some substantial acid hypersecretion. A gastric pH > 2 is mutually exclusive for ZES. Increased serum gastrin levels confirm the diagnosis biochemically. Gastrin secretion can be determined in the basal state or following stimulation with secretin or calcium. High sensitivity and specificity for the diagnosis of ZES is provided by determining the ratio of basal versus pentagastrin-stimulated gastric acid secretion: the ratio of BAO / MAO > 0.6 is highly specific for gastrinoma. To localize the gastrin-secreting tumor computer-assisted tomography, endoscopic ultrasound, and somatostatin receptor scintigraphy provide useful help but most recently, endoscopic ultrasound with high resolution transducers appear to improve preoperative site localization. If modern imaging techniques fail to elucidate the site of the tumor, intraoperative diaphany may help to detect gastrinomas within the duodenal wall.
Tests include:
• Abdominal CT scan
• Calcium infusion test
• Endoscopic ultrasound
• Exploratory surgery
• Gastrin blood level
• Octreotide scan
• Secretin stimulation test
DIFFERENTIAL DIAGNOSES:
Gastrinomas can be associated with Zollinger-Ellison syndrome or Helicobacter Pylori gastritis.
Zollinger Ellison Syndrome
ZES is characterized by a significant hypergastrinemia derived from a gastrin-secreting neuroendocrine tumor with a primary location in the pancreas or duodenum. Chronic hypergastrinemia in turn triggers gastric acid hypersecretion yielding in chronic or recurrent or refractory peptic ulcer disease and/or chronic diarrhea. One half of patients with ZES will have distant metastases in the liver by the time the diagnosis is established and one half of all patients with ZES will experience chronic diarrhea as chief complaint rather than peptic ulcer-related symptoms and signs. Gastrinomas have been reported to either manifest sporadically or to occur in conjunction with the genetic background of the MEN-I syndrome.
Helicobacter Pylori
The 2005’s Nobel Laureates in Physiology or Medicine Robin Warren and Barry Marshall made the remarkable and unexpected discovery that inflammation in the stomach (gastritis) as well as ulceration of the stomach or duodenum (peptic ulcer disease) is often the result of an infection of the stomach caused by the bacterium Helicobacter pylori. HP has been associated with neuroendocrine tumors of the stomach and duodenum too (Grin A, Kim YI, Mustard R, Streutker CJ, Riddell RH. - Source: Departments of Laboratory Medicine and Pathobiology, St Michael's Hospital, Toronto, ON, Canada). Together they found that the organism is present in almost all patients with gastric inflammation, duodenal ulcer or gastric ulcer. Based on these results, they proposed that Helicobacter pylori is involved in the etiology of these diseases. The infection is usually asymptomatic but can cause peptic ulcer. Furthermore, infection is thought to be associated with cancer development, as it slowly induces gastric atrophy, which is known to be a precursor lesion to intestinal metaplasia. Gastric atrophy in response to infection with H. pylori develops slowly over a long period of 20 to 40 years. In some individuals H. pylori results in a more widespread inflammation that predisposes not only to ulcer but also to stomach cancer. There is a clear association between H. pylori and the development of gastric cancer. Therefore, H. pylori was designated as a group 1 carcinogen. However, only approx 0.4% of
the infected population develop gastric cancer.
TREATMENTS:
Definitive treatment will only be achieved by total surgical resection of the gastrin-producing tumor in the pancreas or duodenum including dissection of the regional lymph nodes (Banasch M, Schmitz F. - Source: Department of Medicine I, St. Josef-Hospital, University of Bochum, Bochum, Germany). Control of symptoms will have to be achieved by administration of highly potent proton pump inhibitors in up to 2-3-fold increased standard doses to inhibit gastric acid hypersecretion. Elevation of gastric pH > 4 will be the therapeutic target to protect the mucosa of the upper gastrointestinal tract. Basal acid output should be reduced to less than 10 mEq H(+) per hour which requires administration of highly potent proton pump inhibitors with a recommended starting dose of 60 mg omeprazole equivalents per day.
Medications called proton pump inhibitors (omeprazole, lansoprazole, and others) are now the first choice for treating Zollinger-Ellison syndrome. These drugs reduce acid production by the stomach, and promote healing of ulcers in the stomach and small intestine. They also relieve abdominal pain and diarrhea.
Surgery to remove a single gastrinoma may be done if there is no evidence that it has spread to other organs (such as lymph nodes or the liver). Surgery on the stomach (gastrectomy) to control acid production is rarely needed today.
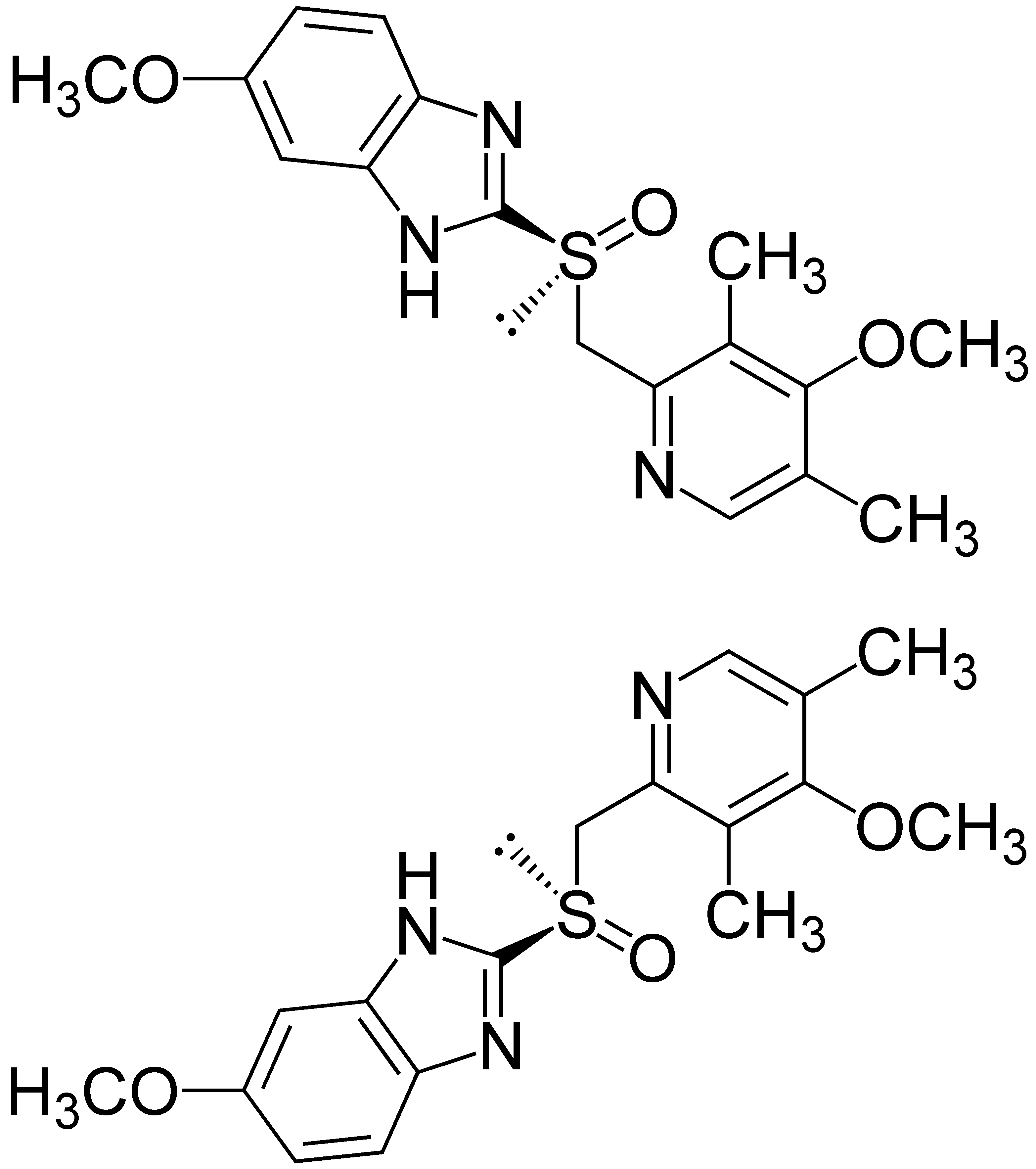
Omeprazole
POSSIBLE COMPLICATIONS:
• Failure to locate the tumor during surgery
• Intestinal bleeding or hole (perforation) from ulcers in the stomach or duodenum
• Severe diarrhea and weight loss
Spread of the tumor to other organs (most often liver and lymph nodes)
CASE REPORT 1
Gastrinoma in a 43-year-old patient with MEN 1 who presented with elevated gastrin levels.
(RadioGraphics March-April 2006 vol. 26 no. 2 453-464)

The patient had a history of nephrolithiasis, hypercalcemia, hyperuricemia, and peptic ulcer disease. Contrast-enhanced CT scan demonstrates a 2-cm exophytic mass (arrow) off the pancreatic tail. The lesion was enucleated laparoscopically. Histologic analysis demonstrated a 3.5-cm ICT. The gastrin levels returned to normal after surgery.