Lanfranco Giacomo
Lauro Alessandro
Resin-Based Composite Biocompatibility
Today, resin-based composite represent one of the most important group of materials in dental practice. They are used in many clinical situations:
- Anterior and posterior filling materials
- Pit and fissure sealants
- Luting composite
- Crown build-ups
- Bonding of brackets and orthodontic bands
- Temporary crown and bridges
- Root canal sealers
Composition
Resin-based filling composite are very complex mixtures containing many substances. These are usually classified into the following groups:
- Filler particles
- Matrix resins and corresponding catalyst systems
- Coupling agents between fillers and matrix resins
Filler Particles have a content that varies between 60-70 vol.%. Mainly consist of finely ground quarz, baron silicate, lithium-alluminum silicate glasses, and highly dispersed amorphous silicon dioxide. Radiodensity is generated by adding special glasses that contain for instance barium, strontium or zinc.
The Matrix resin consists of a mixture of various monomers, for example Bis-GMA and/or UDMA as well as various modifications of these molecules. Other ingredients of the composite matrix are comonomers like EGDMA, DEGDMA and TEGDMA (decreases the viscosity of the matrix) and various additives such as photoinitiators (camphorquinone), o-initiators, inibitors, ultraviolet absorbers, photostabilizers and pigments.
The Coupling between filler particles and matrix resin is obtained through trifunctional alcoxy silanes, which are mostly called Silanes .

To achieve the final structure of the material is fundamental the reaction of polymerization that can be obtained by:
- Exposure to a certain type of light → Fotopolymerizable Composite
- Specific chemical reaction → Autoplymerizable Composite
Resin-based composite are alwais used with the aid of another foundamental materials among which an important role play the Adhesives that often consist of mathacrylates, dimethacrylates, phosphonated penta-acryl esters, acryl amides, aldehydes ( Glutaraldehyde) and organic acids.
Setting Rection
Resin-based composite set through a polymerization of matrix monomers by opening the double bonds at both methacrylate residues of the monomers, thus generating an additive cross-linking. The polymerization of resin-based composites will be either chemically initiated or cured by light initiation. The number of double bonds thet are opened during this process and then participate in the polymerization process is called the Conversion Rate. For resin-based composite, this rate varies between 35% and 75%. An increased solubility of this superficial layer will, of couse, also influence the Biological Properties of the material. Released compounds can directly cause biological reactions. Polymerization shrinkage is a material property that may indirectly influence the tissue compatibility. This volume change may cause marginal gaps that may allow penetration of bacteria with subsequent pulpitis.

Release of Substance
The amount of substance that can be released from resin-based composites is naturally dependent on the extraction medium. More over the composition of the eluates depends on the composition of the resin based composite. The substance segregated from unpolymerized as well as from polymerized resin matrix are:
- Bis-GMA
- Bis-EMA
- UDMA
- TEGDMA (represents the major share of segregated substances)
- EGDMA
- Methylmethacrylate (MMA)
- Filler particles (silicon, boron, sodium and barium)
- Formaldehyde : released into water under certain circumstances; It is very likely generated by an oxidation of unsatured methacrylate groups
- Bisphenol A (BPA): was found in the extract of one pit and fissure sealant and in saliva in contact with resin-based composite. Minute amounts of BPA were detected after placement of UDMA-based and Bis-GMA based composite fillings.
- Fluoride : released from fluoride-containing resin-based composites. However, the clinical caries-prophylactic benefit due to the release of this ion is controversial.
- Adhesives: can also hydrolytically degrade over time, which will result in decreased adhesion. Adhesives’ resin particles were also identified in the pulp.
Sistemic Toxicity
Acute sistemic toxicity was determined by means of LD50 → the calculated dose of chemical substance that kills 50% of the experimental population. Results show that base monomers and comonomers with LD50 of >2,000 mg/kg body weight cannot be classified as toxic. Very few data are available in the dental literature regarding the systemic toxicity of resin-based composites and adhesives.

Estrogenicity
It is well-known from environmental sciences that some chemical substances generate an estrogen-like biological reaction by binding to estrogen receptors of relevant cells at subtoxic concentration → endocrine disruptors. Bisphenol-A (BPA) is one of these compounds. BPA is used in a variety of products, including food and drink containers, CDs and DVDs but also component of a variety of molecules that are present in filling resin composites and pit and fissure sealants. Studies showed consistently that BPA, Bis-GMA and Bis-DMA-containing pit and fissure sealants cause estrogen-like effects. But these effects were generally much smaller than those reactions caused by the control substance, estradiol.
The doses in dental materials are so minute that no clinically relevant estrogen-like effect is expected in patients under physiologic conditions.
Clinical symptoms and complaints
Patients have linked a number of very unspecific symptoms (psycosomatic symptoms or so-called disturbed existential orientation) to resin based composite:
- Insomnia
- Fatigue
- Bronchitis
- Chronic sinusitis
- Depression
- Cardiac arrhythmia etc.
This linking is very difficoult to verify but many studies underline these consequences and the growth of this type of adverse reaction after the use of resin-based composite.
Local Toxicity and Tissue Compatibility
Cytotoxicity
Comprehensive data based on cell culture experiments are available for base monomers of resin-based composites. The citotoxicity of base monomers, expressed by the TC50 (the concentration that causes a 50% reduction of metabolism or cell death) is differnt for each individual substance. Very low concentrations may partly cause a biological reaction. Interestingly, bisfunctional monomers were generally more toxic than monofunctional monomers.

Citotoxicity depends also on:
- Degree of polymerization
- Basic chemistry of the resin matrix ( methacrylate-based materials are more toxic)
- Filler content

Influence on cell metabolism
Composite resin eluates/monomers may interfere with cell metabolism at nonlethal concentrations.

A key molecule in handling nonenzymatic detoxification of substances in the cells is the tripeptid Glutathione (GTH). It is, among others, responsible for mantaining the redox balance in the cell. It was shown that 2-6 h after different cells were exposed to HEMA or TEGDMA, the GSH level decreased, indicating GSH depletion → there was a direct interaction of GSH with the monomers. As a consequence, the intracellular level of reactive oxygen species ROS ( H2O2 , superoxide anion , OH radical ) increased after axposure to HEMA, TEGDMA, or composites resin eluates. However, camphorquinone, after irradiation with blue light used for resin-based composite curing, directly increased intracellular and extracellular ROS concentration → DNA demage via oxidation of DNA bases resulting in single-strand or double-strand breaks has been observed, and DNA demage and chromosome alteration such as the formation of micronuclei have also been described. Dna demage also led to a cell cycle delay in order to give the cell the necessary time to repair DNA demages. Relevant signal molecules for cell cycle delay and DNA repair were activated. If DNA demage cannot be repaired, cell will undergo apoptosis. This may be a consequence of cell cycle arrest or of an activation of the mitochondria-associated caspase-9 pathway by activation of relevant procaspases.
Methacrylates may interfere with cellular cholesterol and phospholipids and thus alter membrane-related functions.
Nuclear factor kappa B ( NFkB ) a key regulator for immunologic reactions including inflammation and regeneration was upregulated by HEMA in primary skin fibroblasts.
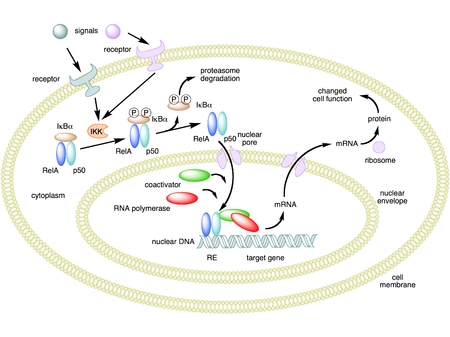
This is in line with the observation that expression of proinflammatory mediators such as interleukin (IL)-6, IL-8 and prostaglandin E2 (PGE2) by epithelial and hematopoetic cells is influenced by TEGDMA exposure. Also blocking (PI 3-kinase) and activating mitogen-activated protein MAP-kinase pathways by TEGDMA increased the NFkB level. Increased NfkBlevels seems to block apoptosis. MAP-kinase are also influenced by TEGDMA and HEMA, and they are involved in tissue regeneration and cell differentiation.
Antimicrobial properties
Resin-based composite hasn’t real antimicrobial activity, many studies show in fact these types di behaviour:
- Resin-based composites and luting composites increase the growth of Streptococcus Mutans
- TEGDMA and EGDMA promote bacterial proliferation of two cariogenic species: Streptococcus Sobrinus e Lactobacillus Acidophilus
- Then composite’s matrix helps adhesion of bacterial microorganisms
Pulp reactions
The Dental Pulp may be damaged by the cavity preparation, specifically in the case of insufficient water cooling, as well as by filling materials. We can see:
- Direct toxic effect = substances that leach from the material
- Indirect toxic effect = the damaging effect due to bacterial toxin subsequent to a microbial colonization of the cavity floor
Biologically active molecules must penetrate from the cavity floor through the dentin to the pulp in order to cause an inflammatory pulpal reaction. However dentin may act as an effective diffusion and absorption barrier. Permeability is lower in dentin distant from the pulp.
No pulp reaction is to be expected in medium-deep or shallow cavities with a comparably thick remaining dentin layer, if penetration of bacteria beneath the filling is avoided → the penetration of potentially toxic substances from shallow or medium-deep cavities to the pulp is overall very low. Comparatively few studies have addressed the effect of resin-based composites or adhesives on the pulp in deep cavities. Human teeth showed istologically pronunced inflammatory reactions after the applications of resin-based composites and adhesives in deep cavities. Small resin particles derived from dentin adhesives were documented in dentin tubules and in pulp, this partcles were surrounded by macrophages, a situation indicative of a foreign body or inflammatory reaction. However, further research on this aspect is necessary.
Moreover this materials are not used in direct capping of the pulp because they often cause the lost of the dental vitality.

We have also to considerate other two important apects of pulp characteristic:
- Thermal effects on the pulp: an increase of 5,5° C of the temperature in the pulp will cause irreversible pulpar demage in 15% of all cases
- Postoperative sensitivity → the possible causes can be: trauma caused by preparation, microleakage with bacterial penetration, polymerization shrinkage and deformation of the restoration under stress

Reactions of gingiva and oral mucosa
Studies showed that gingiva next to sound enamel surface was less inflamed than that adjacent to composite resin fillings, especially in cases in which the fillings ended subgingivally. The degree of inflammation was higher adjacent to resin-based composite fillings compared with amalgams or gold alloys. It can be concluded that reactions of gingiva and periodontium in contact with resin-based composites are probably due to increased plaque accumulation on these materials.

Allergies
Allergies due to dental materials, especially resin-based composite and adhesives, may affect patients and dental personnel as well. Generally resin-based composites and adhesives may cause immediate reactions (Type I) or delayed reactions ( Type IV).
Resin-based composites and adhesives contain a variety of substances that are considered to be allergens. Reports by Danish dentists indicate that 2% of them are suffering from allergic side effects caused by resin-based composites. There is in fact a demonstrated influence of HEMA and other components on immune system.
We can find many simptoms:
- Severe urticaria with skin rashes and swelling on the entire body accrued
- Formation of blisters on child’s face, ears and lips
- Intraorally blisterlike lesions of the gingiva next to the treated teeth

- Swollen lips
- Perioral erythema
- Itching
- Intraoral inflammatory symptoms
- Recurrent Stomatis
- Facial Dermatitis

- Lichenoid reactions of the oral mucosa in direct contact with composite
- Gengivitis (reaction to formaldehyde)

- Asthma
- Rhinitis
- Laryngitis
- Eczemas located on hands

Mutagenicity and Carcinogenicity
In the presence of cholesterol esterase, Bis-GMA formed a degradation product, BADPE-4OH, which then produced micronuclei in cultured human lynphocytes. TEGDMA caused major DNA strand delections and induced micronuclei in mammalian cells ( Chromosomal demage). Glutaraldehyde, which is contained in some adhesives, was mutagenis in vitro. Numeric chromosomal aberration were induced by DMPT (dimethyl-p-toluidine), a frequently used accelerator in catalyst systems.
References
1. Stanley HR.
2. Schmalz, Gottfried, Arenholt-Bindslev, Dorthe
3. Schweikl H, Spagnuolo G, Schmalz G
cosi devono essere le voci bibliografiche e messe dove sono citate, non al fondo
4. Estrogenicity of resin-based composites and sealants used in dentistry. 1996
5. Fung EY, Ewoldsen NO, St Germain HA Jr, Marx DB, Miaw CL, Siew C, Chou HN, Gruninger SE, Meyer DM