Introduction

The rates of depression, anxiety, and sleep disturbance (suicide risk factors) are greater in patients with allergic rhinitis than in the general population. The rate of allergy is also greater in patients with depression. Preliminary data suggest that patients with a history of allergy may have an increased rate of suicide. Clinicians should actively inquire to diagnose allergy in patients with depression and depression in patients with allergy.
Spring peaks of suicide are highly replicated, but their origin is poorly understood. Preliminary epidemiologic data suggest that seasonal spring peaks in aeroallergens are associated with seasonal spring peaks in suicide. A research in Brown Norway rats demonstrates that sensitization and exposure to aeroallergens induces anxiety-like and aggressive behaviors as well as allergy-related helper T-cell type 2 (Th2) cytokine gene expression in the prefrontal cortex. Thus, it is possible that sensitization and exposure to aeroallergens, which peak in spring, may be conducive to seasonal exacerbation of suicide risk factors such as anxiety, depression, hostility/ aggression, and sleep disturbance. Connecting allergy with suicide and suicide risk factors adds to previous neurologic literature connecting allergy with migraines and seizure disorders.
A recent report of Th2 (allergy-mediating) cytokine expression in the orbito-frontal cortex of suicide victims should lead to future studies to test the hypothesis that mediators of allergic inflammation in the nasal cavities may result in Th2 cytokine expression in the brain, influencing affect and behavioral modulation.
Certain medications used to treat allergy can exacerbate suicide risk factors, potentially worsening suicide risk and even triggering suicide. Systemic (but not topical) corticosteroids have been associated with manic and depressive episodes and mixed mood states. Recently, the US Food and Drug Administration started investigating the possibility that montelukast may trigger suicide. Although this association requires further exploration and confirmation, clinicians should err on the side of caution, inquiring about past suicide attempts; hopelessness; reasons for living; and suicidal ideation, intent, or plan; and referring the patient to a mental health professional for evaluation if appropriate.
Allergy, depression and suicide
In 2004, suicide was the 11th leading cause of death in the United States, accounting for 32,439 deaths. For every suicide death, there are an estimated 8 to 25 attempted suicides. Most individuals who complete suicide are depressed. Many short-term and long-term risk factors have been proposed, including socioeconomic factors and psychiatric symptoms and syndromes including depression, anxiety, sleep loss, and aggression. Asthma (with its treatment) is among the many chronic illnesses proposed to increase the risk of suicide, but allergic rhinitis has not made this list in any review or chapter known. The stress-diathesis model, currently one of the most accepted models of suicide vulnerabilities and triggering , proposes that a stressor leads to the exacerbation of a preexisting psychiatric disorder, triggering suicide. A highly replicated finding in epidemiology research is the spring peak in suicide from April to June with a mirror image in the Southern Hemisphere. There is a smaller and less consistent peak of suicide in late summer and early fall. Many factors have been implicated in contributing to the spring peak in depression and suicide, ranging from environmental (light) to social factors, but no single explanation has yet proven satisfactory.
One of the most dramatic environmental changes, which coincides with physical symptoms, is the robust increase in pollen during the spring and the corresponding increased incidence of upper respiratory inflammation. Pollen is the most important and the most seasonal of the aeroallergens. 1. Every year, the air is flooded with pollen from wind-pollinated plants, and the development of allergies due to human exposure is an unfortunate consequence of this process. Tree pollination occurs in the spring and represents the largest source of airborne pollen (∼ 75% of the yearly total). In April, the value typically increases from less than 100 grains/m3 in the first week of the month to more than 1000 to 1300 grains/m3 in the third week. The levels of pollen return to below 100 grains/m3 by the first week of June. The dramatic increase in atmospheric concentration of tree pollen is highly relevant to human health. Another increase in atmospheric pollen occurs during the fall, mainly represented by the pollen of ragweed. Even though ragweed pollen amounts to only about 15% of the yearly pollen total, it is highly allergenic.
Consistent with the hypothesis that allergens trigger suicide in those with a triple vulnerability (ie, for suicide, mood disorders, and allergic reactions) there is a twofold increase in the rate of nonviolent completed suicides among women younger than 65 years during the spring tree allergy season in the high-exposure period compared with the pre-exposure period.

Triple vulnerability for suicide, mood disorders, and allergic sensitization with an environmental trigger (allergen). Mechanisms by which cytokines affect the brain include activation of the hypothalamus-pituitary-adrenal (HPA) axis and the actions of indoleamine deoxygenase (IDO), an enzyme involved in the catabolism of tryptophan (TRP), stealing it from the TRP hydroxylase pathway and serotonin synthesis and producing potentially neurotoxic compounds such as kynurenine (KYN). In addition, several small areas of the brain (the circumventricular organs, CVO) lack a blood-brain barrier and allow larger molecules such as cytokines to interact with neurons, their terminals, and glial cells. BPD—bipolar disorder; MDD—major depressive disorder
This finding is consistent with the findings of Timonen 2. Atopy and depression: results from the Northern Finland 1966 Birth Cohort Study. who reported a greater seasonality of suicide in those with a history of allergy than in those without such a history. One possible explanation for this phenomenon is that one or more of the known suicide risk factors—depression, anxiety, aggression, or sleep impairment—may be affected by exposure to allergens in vulnerable individuals. Marshall et al. 3. Effects of seasonal allergic rhinitis on fatigue levels and mood. used the Multi-Dimensional Fatigue Inventory and the Positive Affect–Negative Affect mood rating scales in patients sensitized to ragweed and reported higher levels of general and mental fatigue (but not physical fatigue), reduced motivation, increased sadness, and reduced pleasurable engagement during the ragweed pollen season as compared with the off-season.
A work in a student population has shown that seasonality of mood is directly related to self-reported sensitivity to pollen counts 4. MOOD-WORSENING WITH HIGH-POLLEN-COUNTS AND SEASONALITY: A PRELIMINARY REPORT.
Finally, is been shown that changes in allergy symptoms from low to high tree-pollen seasons correlate with changes in depression scores 5. Changes in Allergy Symptoms and Depression Scores Are Positively Correlated In Patients With Recurrent Mood Disorders Exposed to Seasonal Peaks in Aeroallergens and anxiety scores in patients with a recurrent mood disorder.
Increasing evidence suggests an association between recurrent depression and allergic diseases 6. Depression and allergies: survey of a nonclinical population..
Neuropsychiatric symptoms associated with allergen exposure.
When exposed to pollen, subjects with allergic rhinitis had decrements in reaction time, attention, and vigilance 7. Decrements in vigilance and cognitive functioning associated with ragweed-induced allergic rhinitis.. Another suicide risk factor, anxiety, has been associated with allergy in women 8. State and trait anxiety in women affected by allergic and vasomotor rhinitis..
Immune function may play a role in depression and suicide 9. Twenty Years of Research on Cytokine-Induced Sickness Behavior..
It is known that treatment of hepatitis C with the cytokine interferon-α, resulting in the reduction of viral titers, induces depression in a significant proportion of patients 10. Neuropsychiatric symptoms associated with hepatitis C and interferon alpha: A review..
A causal relationship between cytokine treatment and depression is further suggested by the cessation of depressive symptoms when cytokine treatments are discontinued 11. Cytokines and depression: the need for a new paradigm..
Moreover, several studies have reported the presence of elevated proinflammatory cytokines in depressed patients and a reduction in these mediators of inflammation after treatment with antidepressants. However, because cytokines induce sickness behaviour, the validity of these studies has been limited by the overlap with the sickness syndrome. Although the degree to which sickness, rather than depression, is involved in these effects is under debate, studies show that healthy individuals receiving low doses of lipopolysaccharides (LPS), components of bacterial cell walls, had elevated anxiety and depressive scores in the absence of sickness behaviour. In animal studies, behaviours that resembled depression and anxiety were induced by activation of the immune system with LPS. These effects have been shown to be mediated by the actions of cytokines in the brain, likely as an adaptive mechanism to cope with potentially lethal infectious agents. Although the involvement of the immune system and cytokines in the pathophysiology of depression has not been fully addressed, it is an active area of research that may contribute to fundamental advances in the understanding of mood disorders. 12. Cerebrospinal cytokine levels in patients with acute depression..
13. Endotoxin- or pro-inflammatory cytokine-induced sickness behaviour as an animal model of depression: focus on anhedonia..
Brain cytokines
An elevated expression of helper T-cell type 2 (Th2) cytokines has been reported in the human orbitofrontal cortex in suicide victims. 14. Elevated cytokine expression in the orbitofrontal cortex of victims of suicide.
Although no data show conclusively that peripheral cytokines can cross the blood-brain barrier, these cytokines can signal cells within the brain through several mechanisms. These include direct actions of circulating cytokines via circumventricular organs, cytokine signalling through the vagus nerve 15. Vagal immune-to-brain communication: a visceral chemosensory pathway.. , de novo transcription of cytokine genes in astrocytes, and microglia induced by inflammatory mediators produced by endothelial cells of the cerebrovasculature.
Several mechanisms have been proposed to explain how cytokines may affect brain function and behaviour. Two of the most important are interactions with the hypothalamic-pituitary-adrenal (HPA) axis and with the indoleamine deoxygenase enzyme. Cytokines can induce activation of the HPA axis 16. Regulation of the HPA axis by cytokines.. , resulting in altered levels of corticotropin-releasing hormone and cortisol with detrimental effects on neurons. Activation of the indoleamine deoxygenase enzyme steals tryptophan from serotonin synthesis toward the production of kynurenines and reduces serotonin production.
Thus, one important mechanism of neuroimmune interactions is the brain's capacity to produce cytokines in response to peripheral immune challenge. This mechanism may change the balance of cytokine expression in the brain and, in turn, may affect neuronal function in response to inflammatory processes initiated in the periphery.
Sleep impairment
Insomnia, hypersomnia, nightmares, and sleep panic attacks are important suicide risk factors. Correcting them may reduce suicide risk relatively swiftly. Proinflammatory cytokines, such as TNF-α, IL-1, IL-6, and interferons, tend to induce sleepiness and sleep 17. Sleep-promoting effects of endogenous pyrogen (interleukin-1).. In contrast, “anti-inflammatory cytokines” have been reported to disrupt sleep. For instance, it has been reported that IL-4 and IL-10 inhibit spontaneous sleep.
18. Interleukin-4 inhibits spontaneous sleep in rabbits. 19. Interleukin-10 inhibits spontaneous sleep in rabbits.
Moreover, in addition to the effects of cytokines, mechanical obstruction secondary to mucosal edema and secretions in the upper respiratory tract could be a direct cause of sleep disturbance and daytime sleepiness and may exacerbate or make manifest obstructive sleep apnea. Intranasal corticosteroids are effective agents in improving sleep in patients with allergy 20. Efficacy of the topical nasal steroid budesonide on improving sleep and daytime somnolence in patients with perennial allergic rhinitis..
Gender effects
A stronger association between allergy, depression, and suicide in women may be explained in part by an increased incidence of allergy and depression in women, or by increased anxiety associated with depression in women. To a certain degree, the effects could be hormonal. Specifically, beta-estradiol and progesterone significantly increase the production of IL-4 and IL-13 21. Effect of sex hormones on eosinophilic inflammation in the nasal mucosa.. , whereas testosterone inhibits histamine release and eosinophil d egranulation. Estrogens favour a Th2 IgE–mediated response, which may explain, in part, the increased prevalence of the allergic disease in women of reproductive age as compared with men.
Intranasal-intracanial comunication
As much as the brain is (incorrectly) considered an “immune-privileged organ,” the relationship between the nasal cavity and the brain is also a “privileged” and “intimate” one. First, the nasal cavity is the only place in which central nervous tissue (ie, the olfactory neurons) is directly exposed to air carrying chemicals, pathogens, pollutants, and allergens. Second, the transfer of large molecules and pathogens into the brain via the intranasal pathway has been reported. It is important to mention that the intranasal pathways may, via olfactory and trigeminal pathways, deliver large molecules into brain areas that play a key role in mood regulation and dysregulation more efficiently than intravascular administration 22. Delivery of insulin-like growth factor-I to the rat brain and spinal cord along olfactory and trigeminal pathways following intranasal administration..
In addition, it has been shown that intranasal instillation of recombinant cytokines, including IL-6 and IL-12, affects the course of experimentally induced neurologic disorders in rats 23. Intranasal administration of human IL-6 increases the severity of chemically induced seizures in rats..
Allergic rhinitis: clinical considerations
Allergic diseases affect 10% to 30% of adults and nearly 40% of children and are increasing in prevalence for unknown reasons. Symptoms of allergy are occasionally life-threatening, sometimes debilitating, and frequently very bothersome. In the lungs, allergy is manifested by bronchoconstriction or asthma; in the nose, by rhinitis; in the skin, by urticaria; and in the eyes, by conjunctivitis. Anaphylaxis—the systemic and life-threatening manifestations of allergy—requires immediate medical attention. In contrast to allergic rhinitis, asthma is often treated with systemic corticosteroids, which may themselves cause neuropsychiatric symptoms. Because of anatomic proximity inflammation of the nasal cavities may have a closer relationship with the brain than inflammation of the skin, lungs, or digestive tract. The distinction between asthma and nasal inflammation is somewhat illusory, however, because more than 60% of individuals with rhinitis also have asthma, and allergic rhinitis frequently progresses toward allergic asthma.

Rhinitis symptoms include rhinorrhea, nasal congestion, sneezing, itching of the nose, postnasal drainage, or a combination of these. Allergic rhinitis also is often associated with symptoms of allergic conjunctivitis, including tearing, redness, ocular itch, and sometimes swelling and photophobia. In addition to allergic variables, irritant, infectious, hormonal, occupational, and other factors may predispose individuals to rhinitis or may trigger or aggravate it.
Peak presentations of allergic rhinoconjunctivitis occur between ages 10 and 25 years. Rhinitis has traditionally been classified as “seasonal” or “perennial,” but recently there has been a tendency to classify rhinitis as intermittent (≤ 4 days per week or, if > 4 days per week, then total duration of < 4 weeks) or persistent. Allergic rhinitis is classified as moderate/severe rather than mild if symptoms are severe or if they result in impairment of sleep, daily activities, work, or school.
Research
Animal studies, as an immediate priority, can test the effect of medications used to treat allergy in behavioural analogues of suicide risk factors (eg, aggression, behaviours resembling depression or anxiety, impulsivity, sleep impairment) at baseline and after sensitization and exposure to antigens. Animal studies also can elucidate mechanisms of transmission of inflammation from the nasal cavity to the brain and test mechanisms of interventions. Larger postmortem studies with better controls are needed to localize the cellular substrate of Th2 inflammation in the brain using in situ hybridization. Large-scale clinical trials could compare the effect on suicide risk factors of intranasal corticosteroids, antihistamines, and leukotriene inhibitors in patients with recurrent mood disorders (preferably those with a history of suicide attempts). Functional neuroimaging studies are needed to determine brain activity changes with exposure to aeroallergens in sensitized individuals stratified by diagnosis of mood disorders and suicide attempt history (number, severity). Epidemiologic studies are needed to study completed suicide; for replication, it is essential to confirm a relationship between suicide (completed and attempted) and prior history of allergy and timing of exposure to allergens, ideally with adjustment for history of mental and medical illness and socioeconomic factors previously implicated in suicide.
Pathophysiology
Certain individuals with an atopic predisposition synthesize IgE antibodies upon initial exposure to an allergen. IgE binding to mast cells and basophils sets the stage for the allergic response. Upon re-exposure, the allergen binds and crosslinks IgE bound to the cell surface, resulting in the release of inflammatory mediators. Early response mediators include lipid mediators (leukotrienes, prostaglandins) and granule mediators (histamine, tryptase).

Minutes to hours later, cytokines such as TNF-α, IL-4, IL-5, and IL-6 and chemokines (IL-8, monocyte chemotactic protein-1, macrophage inflammatory protein-1α) are released [88, Class II]. The type of allergen, the degree and length of exposure, and the atopic tendency of the individual determine the manifestation of symptoms. Allergen contact occurs via the air (seasonal aeroallergens tree, grass, and weed pollen and perennial dust mite protein, animal dander, and mold), food, drugs, and skin (stinging insects).
Allergic rhinitis pathophysiology is characterized by oedema of the nasal mucosa as a result of IgE-mediated release of early-phase and late-phase mediators and Th2 cytokines, which promote the infiltration of mucosa with inflammatory cells: eosinophils, neutrophils, basophils, T cells, and macrophages.
Diagnosis
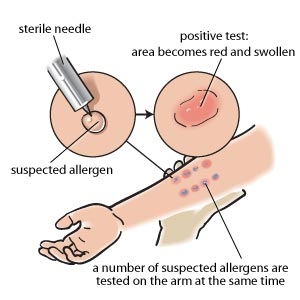
In addition to the symptoms of allergy, in vivo and laboratory-based testing for allergen sensitivity may objectively support the diagnosis of allergic disease. Skin prick and intradermal testing measure IgE-mediated hypersensitivity in the skin, quantifying the wheal and flare response within 15 minutes of allergen contact. The skin prick and intradermal testing lose their value if skin response is decreased through treatment with antihistamines, antihistaminic effects of other medications (including many psychotropic agents), or increased skin sensitivity from dermatographism. In that case, specific IgE antibodies may be detected in serum with comparable sensitivity and specificity.
Treatment
There are no current data on the treatment of allergic rhinitis in individuals with a history of neuropsychiatric conditions. Nevertheless, good management of nasal inflammation may be very important for the general management of neuropsychiatric conditions, specifically recurrent mood disorders with an increased risk for suicide. The general principles of treatment are given here. Future studies ideally will successfully focus on the treatment of allergic rhinitis in patients with depression, the treatment of depression in patients with allergic rhinitis, and the effects on specific suicide risk factors of each medication from the antiallergy arsenal.
Diet and lifestyle
Minimize contact with allergens. Avoid outdoor exposure when aeroallergen counts are high.
Reduce the aeroallergen load to the mucosa. Saline nasal irrigation is a safe and effective method of cleansing the nasal mucosa of allergens and improving sinus symptoms 24. Clinical study and literature review of nasal irrigation.
Reduce allergen load in microclimates. Vacuum cleaning, furnace filters, dehumidifiers, “allergy bedding,” and washing bed linens in hot water may reduce exposure to dust mites (the most important perennial allergen) and other perennial allergens.
Pharmacologic treatment
Drug therapy for allergic rhinitis has many aims: stabilizing mast cells, reducing the effects of histamine, reducing inflammation, reducing secretions, reducing the production and effects of inflammatory mediators, reducing activation of prostaglandin pathways, maintaining the patency of sinuses and lacrimal channels, treating pain from a sinus infection, and desensitization.
Clinicians should ask about depression, anxiety, and sleep disturbance, and treat them if present.
Clinicians also should ask about suicidal ideation and consider whether medications the patient is taking are increasing the risk of suicide. Referral for evaluation of suicide risk and preventive treatment may be appropriate.
Drugs used to treat allergic rhinitis include decongestants (oral and intranasal), antihistamines (oral and intranasal), corticosteroids (intranasal, rarely oral or parenteral), cromolyn (intranasal), anticholinergics (intranasal), and some newer combinations.
Pharmacologic treatment of allergic diseases related to mental health