NICKEL HYPERSENSITIVITY (Andrea Garnero and Ilaria Peluttiero)
DEFINITION
Nickel
Nickel allergy is an inappropriate reaction of the immune system to the substance nickel. It is one of the most common forms of allergic contact dermatitis in which skin gets inflamed due to contact with an allergy causing substance.
Systemic contact dermatitis is seen when sensitized individuals are exposed to a hapten systemically, that is orally, transcutaneously, intravenously, subcutaneously, intramusculaly or by inhalation.
The most specific cutaneous reactions of systemic contact dermatitis include flare-up reactions in previously positive patch test sites and/or flares of previous sites of contact dermatitis. Other clinically characteristic cutaneous features are vesicular hand eczema, eruptions on previously unaffected skin such as flexural dermatitis, maculopapular rash and vasculitis-like lesions. Itching and general symptoms, such as headache, nausea and malaise, have been reported after the oral nickel exposure of nickel-sensitive individuals.
Nickel allergy is commonly associated with earrings and other jewelry for body piercings (Jewelry Allergy - Nickel Allergy).
But we can find nickel in a huge quantity of things: foods, coins, stainless steel cookware... (Where is Nickel Found?)
Although systemic contact dermatitis from medicaments is a well-established entity, the existence of systemic reactions to oral nickel exposure, in particular systemic reactions to nickel exposure in the normal daily diet, remains controversial.
EPIDEMIOLOGY
Nickel allergy can affect people of all ages. Nickel allergy is more common in women, probably because they are more likely to have pierced ears than men, although this is changing.
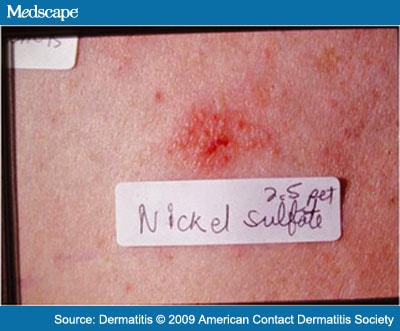
Allergy to nickel is a phenomenon which has assumed growing importance in recent years, largely because of the introduction of cheap fancy jewellery in which the underlying metal layer consists of nickel. 10 to 12% of the female population and 6% of the male population are estimated to be allergic to nickel. In fact the allergy is not caused by nickel itself but by the nickel sulfate NiSO 4 (H 2 O) 6 , which are formed under the effect of perspiration in contact with the piece of jewellery or watch. This phenomenon is always accompanied by corrosion of the object.
SYMPTOMS
The most specific cutaneous reactions of systemic contact dermatitis include flare-up reactions in previously positive patch test sites and/or flares of previous sites of contact dermatitis. Other clinically characteristic cutaneous features are vesicular hand eczema, eruptions on previously unaffected skin such as flexural dermatitis, maculopapular rash and vasculitis-like lesions. Itching and general symptoms, such as headache, nausea and malaise, have been reported after the oral nickel exposure of nickel-sensitive individuals.
Allergic contact dermatitis defined as a T-cell-mediated delayed-type skin hypersensitivity response to low molecular weight substances, represents a considerable environmental and occupational health hazard in developed countries. Relevant agents causing occupation-induced ACD comprise the ubiquitous transition metal nickel (Ni ++).
DIAGNOSIS



The physician can usually diagnose nickel allergy based on:
* skin's appearance
* recent history of contact with items that may contain nickel
* If the cause of the rash isn't apparent, however, the physician may recommend a patch test (contact hypersensitivity allergy test).
During a patch test, very small quantities of potential allergens (including nickel) are applied to small patches, which are then placed on your skin to check for a reaction. The patches remain on your skin for two days before the doctor removes them. If you have a nickel allergy, the skin under the nickel patch will be inflamed when the patch is removed or in the days after removal of the patch. Because of the low concentrations of allergens used, patch tests are safe even for people with severe allergies.
PATHOGENESIS
Contact allergy requires cooperation of adaptative and innate immunity.
Ni ++ stimulates innate immunity via TLR4/MD2, the bacterial LPS receptor. Recently, it was demonstrated that human Toll-like receptor 4 (TLR4), an innate immune receptor detecting bacterial lipopolysaccharide (LPS), has a crucial role in Ni ++ -mediated inflammatory reactions. On the basis of structural modelling and mutagenesis data we proposed a model, in which two Ni ++ ions bind a histidine triplet provided by two opposing TLR4 molecules. Similar to LPS, Ni ++ thus might induce proinflammatory signaling by crosslinking two TLR4 molecules.
( Metal allergens nickel facilitate TLR4 homodimerization indipendently od MD2, Badrinarayanan Raghavan et al.2012)
It has been suggested that ACD can be distinguished from other skin disorders like psoriasis and atopic eczema by the specific profile of Th cell subsets involved and Th17 and Th22 were detected in skin lesions of allergic individuals.
In addition to other costimulatory molecules such as CD86, programmed death ligand (PD-L)1 (B7-H1, CD274) and PD-L2 bind to their cognate receptor PD-1 on activated T and B cells, thereby modulating and fine tuning the balance of immune responses toward pathogens and autoimmune tissue damage. PD-L1 controls the T cell stimulatory potential by limiting IL-2 and IFN-γ release.
PD-L1 tissue expression was analyzed by immunohistochemistry in tissue biopsies taken from ACD patients after nickel exposure. By fluorescence microscopy, PD-L1 expression was found greatly enhanced upon challenge with nickel. At the 72 hours time point the majority of cells constituting epidermal layers exhibited strong expression of PD-L1. By contrast, comparably low PD-L1 levels were observed in biopsies of unchallenged ACD patients (time point: 0 h).

Data on LC-Th cell interactions suggest that PD-L1 expressed on the surface of LCs plays a regulatory role in skin`s immune response to bacteria and in ACD by limiting the release of proinflammatory cytokines from Th cells.
Nickel induces release of IL-22 and TNF-α after blockage of PD-L1.
( Human Langerhans Cells Control Th Cells via Programmed Death-Ligand 1 in Response to Bacterial Stimuli and Nickel-Induced Contact Allergy, Hitzler et al.2012 )
ANATOMICAL TISSUE SPECIFIC RISK FACTORS
Contact sensitization is frequent in the general population and arises from excessive or repeated skin exposure to chemicals and metals. However, little is known about its genetic susceptibility.
A cross-sectional study has been set to determine the role of polymorphisms of the claudin-1 gene (CLDN1) on the risk of contact sensitization, taking common filaggrin gene (FLG) mutations into account.
In individuals without ear piercings, a higher prevalence of nickel sensitization was found in those with the minor allele of CLDN1 SNP rs9290927.
For CLDN1 rs17501010, contact sensitization to organic compounds was associated with the major allele. The risk pattern was also identified for self-reported nickel dermatitis.
In short, the CLDN1 polymorphisms rs9290927 and rs17501010 were associated, respectively, with nickel contact sensitization in individuals without ear piercings and with both organic compounds and nickel contact dermatitis.
The risk of allergen penetration is determined not only by dose and exposure time, but also by the chemical properties of the contact allergens in question, as well as the presence of irritants. In a recent review article, the stratum corneum, tight junctions and dendritic cells were referred to as ‘the three musketeers’ of the epidermal barrier due to their crucial role in skin homeostasis.
The tight-junction barriers exist covertly under the stratum corneum and divide two adjacent compartments to maintain different solute concentrations.
As the tight-junction barrier may be regarded as a second line of defence, CLDN1 mutations could have an impact on the susceptibility to develop contact sensitization and dermatitis. Even though CLDN-1 is just one of several tight-junction proteins, it is a key component of the epidermal protein structures. Absence of CLDN-1 is implicated in neonatal sclerosing cholangitis associated with ichthyosis, and it has been suggested that hypomorphic CLDN1 mutations are responsible for related mild
phenotypes. Provided that an inherited impairment of the stratum corneum, e.g. due to FLG mutations, causes increased allergen penetration of ‘the first line of defence’, one would also expect increased effects of a concomitant leaky ‘second line of defence’ due to genetic variation in the tight junctions. However, we could not confirm an increased effect of CLDN1 polymorphisms when FLG mutations were present. It must be underscored that the numbers in the subanalyses were often small and that the results therefore should be interpreted with caution.

RISK FACTORS
DIRECT CONTACT
Nickel is a very common cause of allergic contact dermatitis (ACD). Sensitized individuals generally have a predictable localized response following cutaneous exposure to nickel, including erythema, vesicles, scaling, and pruritus.
The EU nickel directive states legal limits for the amount of nickel released by items that are normally in prolonged contact with the skin, such as earrings or watches.
Nickel Directive
Annex I to Directive 76/769/EEC
Annex I to Directive 76/769/EEC
Nickel and its compounds may not be used:
1. in post assemblies which are inserted into pierced ears and other pierced parts of the human body during ephitelization of the wound caused by piercig, wheter subsequently removed or not, unless such post assemblies are homogeneous and the concentration of nickel – expressed as mass of nickel to total mass – is less than 0,05%;
2. in products intended to come into direct and prolonged contact with the skin (such as earrings, necklaces, bracelets and chains, anklets finger rings, wrist-watch cases, watch straps and tighteners, rivet buttons, tighteners, rivets, zippers and metal marks, when these are used in garments) if the rate of nickel release from the parts of these products coming into direct and prolonged contact with the skin is greater than 0,5 µg/cm2/week;
3. in products such as those listed in point 2 where these have a non-nickel coating unless such coating is sufficient to ensure that the rate of nickel release from those parts of such products coming into direct and prolonged contact with the skin will not exceed 0,5 µg/cm2/week for a period of at least two years of normal use of the product
Furthermore, products which are the subject of point 1, 2 and 3, may not be placed on the market unless they conform to the requirements set put in those points.
It is not routinely used to test coins: euros break the European Union's own rules. The currency, adopted by most of Europe at the beginning of this year, can release up to 320 times the amount of nickel that European Union (EU) regulations say triggers skin reactions in people allergic to the metal.
This is one of the highest rates of nickel release ever measured for any coins. Frank Nestle of the University of Zurich in Switzerland and colleagues have now worked out why - and it's not just that the new coins contain too much nickel.
In a sweaty palm, each coin is like a tiny battery, Nestle's team shows. When sweat gets between the two different alloys of the central pill and outer ring of 1- and 2-euro pieces, metal ions flow between them. This makes the coins corrode, releasing nickel ions, which can set off itching and redness in up to 30% of the population.
( Nature: High nickel release from 1- and 2-euro coins )
DIETARY NICKEL
Systemic reactions, such as hand dermatitis or generalized eczematous reactions, can occur due to dietary nickel ingestion.
Dermatitis resulting from dietary nickel has been demonstrated in multiple studies. Jensen et al.2003 showed dose-dependent relationships between the amount of nickel ingested and the probability of a dermatitis flare and between the amount ingested and the severity of flares. Doses of 0.3mg, 1mg, and 4mg of nickel sulfate hexahydrate produced cutaneous reactions in 40, 40, and 70 percent of nickel-sensitive participants, respectively. Sixty percent of the participants receiving 4mg of nickel sulfate hexahydrate had widespread cutaneous reactions; whereas, the rate in the placebo group was zero percent.
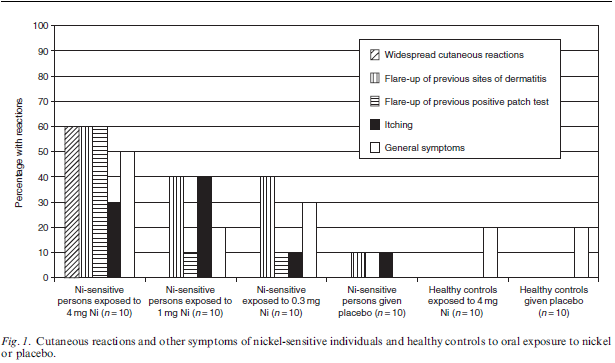
This figure shows the distribution of volunteers with specifically nickel-related cutaneous reactions, as well as itching and general symptoms. The result of the logistic regression analysis showed that the nickel-related reaction pattern seen among the nickel-sensitive volunteers was dose dependent (P=0.021). The frequency of reactions among nickel-sensitive volunteers exposed to 4.0 mg nickel was statistically significantly different from the frequencies in the group given a placebo (P=0.0099) and from the equivalent control group (P=0.0015). Only the nickel-sensitive individuals in the group exposed to 4.0 mg nickel had a significantly different response frequency compared to the other groups (P=0.029 and 0.0054). A significant difference (P=0.016) was seen only when the nickel-sensitive individuals exposed to 4mg nickel were compared with the nickel-sensitive individuals given a placebo.
There are two primary situations in which dietary nickel should be considered as a possible cause or exacerbating factor of dermatitis.
The best known situation is vesicular hand dermatitis in which there is a positive patch test reaction to nickel.
The second, less known situation, is that of a widespread dermatitis or even isolated pruritus in the setting of a positive nickel patch test. Dietary nickel reactions should be particularly strongly considered when papules on the extensor elbows are noted in patients with widespread dermatitis or hand dermatitis. This relationship between systemic contact dermatitis due to dietary nickel and an eruption on the extensor elbows has been shown to be significant. However, since many patients with dermatitis or itching due to dietary nickel do not have this sign, its absence should not dissuade the astute clinician from suspecting the diagnosis of dietary nickel dermatitis.
Nickel ingestion causes detectable changes in the immune system that may explain the observed clinical reactions. For example, ingestion of nickel leads to a decrease in circulating CD8+ CD45RO+ CLA+ blood lymphocytes, which correlates with migration of CD8+ memory T cells into tissues. Ingestion of nickel by nickel-sensitive patients has also been shown to increase serum levels of interleukin (IL)-5, a Th2 cytokine, and although contact dermatitis is classically thought of as a type IV hypersensitivity (Th1 reaction), IL-5 is known to enhance proliferation of eosinophils and may explain why eosinophils can be seen on biopsy.
In addition to the specific foods eaten, a number of other factors can affect the nickel content in the diet. Nickel levels in a given type of fruit or vegetable can vary based on region, water supply, and soil conditions. Nickel can be inadvertently added to processed foods based on the equipment used for processing and can be added to canned foods via leaching from the metallic can. Nickel is also present in tap water, especially hot water, which can leach nickel from faucet fixtures into the water sitting overnight in the fixtures. Stainless steel cookware is another potential dietary nickel source since cooking acidic foods, such as tomato, vinegar, or lemon in stainless steel cookware has been shown to leach nickel from the cookware into the food.
The final, and probably least appreciated, factor in the effects of dietary nickel is absorption of ingested nickel. It has been demonstrated that vitamin C decreases absorption of dietary nickel, as does iron. Co-ingestion, or lack thereof, of these two nutrients can have a major effect on nickel absorption, even without alteration of the amount of nickel ingestion. Factors such as these highlight how little is understood about the ingestion and metabolism of dietary nickel and the factors that can affect it.
THERAPY
Initially, the affected area should be thoroughly washed to remove any residue of the irritant that may remain on the skin.
Cool compresses applied to affected areas may help relieve itching, swelling, and redness. Antihistamines may be used to improve allergy symptoms, including red, itchy and inflamed skin. Commonly used non-prescription antihistamines include diphenhydramine, chlorpheniramine and loratadine among others. Commonly used prescription medications include desloratadine, fexofenadine and cetirizine among others. Emollient creams also known to act frequently to relieve itch and dry skin.
Topical steroids may also be advised for this allergy. In severe cases, systemic steroids may be given to ease inflammation. Antibiotic creams or pills such as penicillin antibiotics may be administered for secondary infection.
Ironically, there is no known and proven treatment for this form of allergy. The above explained measures provide relief to the annoying symptoms and secondary problems related to allergy but are of no great help in providing a permanent cure to the allergy. Even desensitization techniques, such as allergy shots are not an effective modality of treatment, therefore avoidance of nickel is probably the best defence.
A low nickel diet has been shown to be effective in multiple studies. This diet is inexpensive, and there are no known significant side effects of the diet. However, the low nickel diet is relatively fiber poor and can lead to constipation in some patients. The authors recommend fiber supplementation for patients who are on this diet. Disulfiram, a nickel chelator, has been shown to be useful as well, but due to the potential for hepatotoxicity in patients taking disulfiram, this medication is probably best reserved for patients with a high suspicion of dietary nickel dermatitis who have failed a low nickel diet. Alternative ways to decrease dietary nickel absorption (and promote fecal excretion) are to recommend addition of iron-rich foods to the diet since iron is a competitive inhibitor of nickel absorption and to recommend vitamin C supplementation, as vitamin C has been shown to reduce the rise in plasma nickel concentration when ingested concurrently with nickel.


In 2007, Sharma proposed nine points important in achieving a low nickel diet. Using Sharma’s points and the available literature as a guide, the authors of this review agree with the following simplified recommendations: (1) avoid or moderate high nickel foods, canned foods, and vitamin supplements/drinks with nickel; (2) eat high vitamin C- and iron-containing foods; (3) run tap water for a few seconds before washing, drinking, or cooking to flush out nickel that may have leached from pipes or fixtures; (4) avoid stainless steel cookware and utensils when cooking acidic foods; (5) consider vitamin C and/or iron supplementation with meals.
( Sharma's points for a low nickel diet )
CONCLUSIONS
Skin exposure to contact allergens is practically impossible to avoid due to their frequent use in consumer and occupational products. Identification of the critical determinants of interindividual variation of sensitization and elicitation threshold levels may ultimately improve prevention, as genetically susceptible individuals may be instructed to take particular precautions. GST gene polymorphisms have previously been associated with contact sensitization and other inflammatory disorders whereas CLDN1 polymorphisms have been associated with atopic dermatitis in a case–control study.
The literature and experience clearly demonstrate that some nickel-allergic patients have cutaneous reactions when they consume a high nickel diet and that reduction of dietary nickel intake can cause improvement in these patients. Proper dietary modification is harmless and is very inexpensive. For these reasons, recommendation of a low nickel diet should be considered for all patients with either hand dermatitis or a nonspecific, pruritic dermatitis and a positive patch test reaction to nickel.