Enrica Camerino & Greta Cena
Introduction
Sometimes, people affected by cardiac arrest died in mysterious circumstances; some researches (Death caused by cardioinhibitory reflex cardiac arrest--a systematic review of cases, 2011; Traumatic carotid sinus reflex death, 1989) show that in these cases, the death can be due to a mechanism, the cardioinhibitory reflex cardiac death, which causes a reduction in blood pressure and heart rate, cerebral hypoperfusion, reduction of the peripheral vessel tone and loss of consciousness that leads to terminal cardiac arrest.
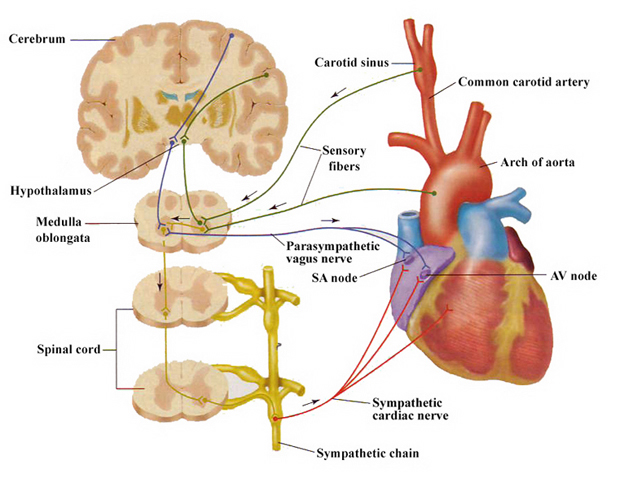
The cardioinhibitory reflex cardiac death consists in a hyperstimulation of carotid sinus, a group of baroreceptors localized in a dilation of the internal carotid artery that have homeostatic functions, which is sent to the cardiorespiratory centers (nucleus tractus solitarius, NTS) in medulla oblongata (via glossofaringeal nerve) and then to the brain; from here, parasympathetic fibers carried the instruction back to the cardiorespiratory centers, and then to the nucleus ambiguus where they contract synapse with the vagus nerve that innervates the sinoatrial and atrioventricular nodes, reducing the heart rate (Vagus nerve stimulation-induced bradyarrhythmias in rats, 2009; Vagus nerve stimulation decreases left ventricular contractility in vivo in the human and pig heart, 2001).
This reflex could explain the deaths occurred after strangling, chocking game (especially in teenagers) or autoerotic strangulation and also in case of violence against the neck without the aim of killing the victim.
It is possible to manually stimulate the carotid sinus ( carotid sinus massage ) and this happens in several occasions like shaving or, more often, when the necktie is tied too much tightly; moreover, even a mild stimulation of baroreceptors can lead to an exaggerated response of carotid sinus if the person is affected by carotid sinus hypersensitivity.
Molecular mechanism
The baroreceptors are activated by stretching and by the rising blood pressure, which close potassium channel causing depolarization of the cell membrane; this leads to the opening of voltage-gated calcium channel that allows calcium to enter in the cell. The rise of intracellular calcium concentration causes the exocytosis of vesicles containing various kinds of neurotransmitters, such as acetylcholine and noradrenaline, which flow across the synapse and cause an action potential that moves to NTS. The NTS sends inhibitory fibers to the sympathetic nervous system and other excitatory fibers to nucleus ambiguus, thus stimulating the parasympathetic nuclei of vagus nerve; the excitation is transmitted to the axons and causes the exocytosis of vesicles of acetylcholine. Acetylcholine binds to muscarinic receptors M2 in the heart and actives a G protein that opens a potassium channel, allowing the efflux of this ion from the pacemaker cell; moreover, the activated M2 receptor decreases intracellular cAMP, slowing the opening of calcium L channels (Muscarinic modulation of cardiac activity, 1999), and also closes calcium T channels through an inhibitory G protein. So, acetylcholine decreases the frequency of pacemaker action potential and leads to bradycardia.


Pathophysiology of carotid sinus hypersensitivity
While the physiology of the normal carotid baroreflex is reasonably well established, the pathophysiology of carotid sinus hypersensitivity (CSH) remains obscure.
The factors that may facilitate CSH are:
- Gender: males are more likely to develop Carotid Sinus Hypersensitivity;
- A sudden feeling of dizziness or disorientation when one stands up quickly (orthostatic hypotension); this is a result of low blood pressure at the particular time when one stands up from a sitting position;
- Age related: the chances of developing this condition increase with age; CSH is more prevalent in the elderly generation and predominantly affects those over the age of 50;
- The presence of atherosclerotic plaques or coronary artery disease or heart disease can make one more susceptible to CSH;
- Tumors in the head or neck region;
- The presence of high blood pressure;
- Certain medications, like beta-blockers or methyldopa, can make ones carotid sinus more sensitive;
- It has been proposed that central a2 adrenoceptor upregulation provides the substrate for the changes in baroreflex gain which manifest as CSH. This hypothesis suggests that carotid sinus stiffness resulting from age-related cardiovascular disease causes relative diminution of afferent baroreceptor neural traffic, with compensatory brain stem post-synaptic a2 adrenoceptor upregulation. This physiologic denervation hypersensitivity then causes the overshoot bradycardia and hypotension following carotid sinus stimulation that is clinical CSH. Though widely quoted, this hypothesis has no evidence base (Central a2 adrenoceptors and the pathogenesis of carotid sinus hypersensitivity, 2004);
- Studies have shown that the affection of the heart rate and blood pressure by pressure of the carotid bifurcation occurs only under certain conditions; in a few cases, ventricular fibrillation was induced, but in these cases the condition of increased hypersensitivity of the carotid sinus was present, due to pre-existing cardiac arrhythmia and digitalis medication. An increase in the carotid sinus activity (hypersensitive carotid sinus), occurs from the age of 40 and from the age of 60 also with asystolia. The reason for the increased carotid sinus activity is the age-dependent developing of atherosclerosis of the carotid vessel wall.
In case of pressure on the carotid bifurcation, the baroreceptors in the internal carotids are pushed against the atherosclerotic plaques; this way, atherosclerotic alterations and diseases that promote atherosclerosis (like hypertension in diabetes mellitus) lead to a hypersensitive carotid sinus. Moreover, space consuming tumors of the head and neck, which press on the carotid bifurcation as well as jaundiced disease and medication (insulin, digitalis), can increase the reflex activity of the carotid sinus; on the other hand, alcohol may reduce the sensitivity.
The susceptibility of the carotid sinus is of considerable importance; Franke revealed in a study with 3500 persons that in 9% of all cases a hypersensitive carotid sinus was present (Cardioinhibitory carotid sinus hypersensitivity: prevalence and predictors in 502 outpatients, 2008);
- A significant anatomical variation in the location of the carotid sinus was measured: most of carotid bifurcations (CB) were found at the level of C3. The vertebra level of CB was differently distributed in distance of the whole neck between upper borders of C1-C2 to lower border of C5 (Morphological Variation of the Carotid Sinus Location, 2012); 54% of the level of CB was asymmetrical between the right and left side. This variation was found to have an impact on the pressure transmission at the carotid sinus region in those individuals that displayed the superior/inferior range of carotid sinus loci; the pressure stimuli would not be located over the locus of the carotid sinus.
Diagnosis and treatments for CSH
There are some symptoms that help the doctor to make a diagnosis of CSH:
- Frequent dizzy spells;
- Low blood pressure;
- A loss of muscle tone at times due to a decrease in heart beat and blood reaching the muscles;
- Excessive scarring in the neck region due to a trauma or the development of fibrosis and neck tumors in this area;
- Flat lining or having no heartbeat for a period of time;
- Forgetfulness or amnesia after an event which leaves one unconscious;
- A slow heart beat or one that beats under 60 beats per minute;
- Sudden falls which can result in injuries and fractures in elderly subjects (Carotid sinus syndrome and falls in older adults, 2001);
- Sudden death or strokes;
- Carotid sinus reflex death is a result of vagus nerve impulses which may cause the heart to stop beating, i.e. cardiac arrest; this occurs during strangulation.
However, in many cases a person may be completely symptom free or asymptomatic and still have CSH.
The CSH is often diagnosed when one experiences unexplained dizziness and disorientation; the doctor can also use massage techniques in the neck region while monitoring any drop or fall in the blood pressure. The possibility of Cardiac arrest should also be monitored.
Treatments for CSH include:
- Denervation surgery: it is a procedure which helps prevent nerve impulse responsiveness and conductivity;
- Endarterectomy, a surgical procedure which helps remove plaque or plaque build-up in the arteries; if this plaque becomes dislodged it can get stuck in narrow arteries causing a blockage and prevention of blood flow in this area;
- Medications such as Heparin, Asprin and Plavix are recommended to prevent blood clotting and thickening of blood; these are known as anticoagulants.
Moreover, a person who suffers from CSH should:
- Avoid massaging of the carotid sinus; this can be very dangerous, especially in people affected by atherosclerosis, as any massaging to this area can cause a thrombus or plaque to become dislodged resulting in it flowing freely through the arteries with a possibility of becoming lodged in a narrow artery and resulting in strokes and even death;
- Avoid wearing tight fitting collars or neckties;
- Try decreasing the speed at turning the head;
- Be careful when shaving over this artery as not to over stimulate it.
Therapeutic effects
Carotid sinus massage (CSM) is a simple bedside maneuver that helps to clarify the type and sometimes also the mechanism of different rhythm disturbances; the major indication for CSM is the diagnosis of tachyarrhythmias in which the atrial activity is either absent or intermittently present, but it is also used in some patients with normal heart rates or for evaluating the function of permanent pacemakers (Carotid sinus massage. Its diagnostic and therapeutic value in arrhythmias, 1985).
CSM is also an important diagnostic procedure in patients with suspected CSH, especially for those subjects over 40 years with unexplained syncopes (Age indications for carotid sinus massage: a case for maintaining the status quo?, 2009); the response to CSM is affected by the patient's position, and in patients with unexplained syncope or drop attacks, upright CSM is recommended if initial supine CSM is not diagnostic.
Time of day at which massage is performed is usually not taken into consideration, even if the diagnostic and therapeutic value of CSM may vary according to circadian rhythm (Effect of circadian rhythm on response to carotid sinus massage, 2001).
Alterations in vagal tone can influence the atrial fibrillatory process by changing the atrial refractory period; a study shows that in a patient with paroxysmal atrial fibrillation (AF) the CSM changed a "coarse" type of fibrillation into a "fine" type, followed by termination of the arrhythmia (Carotid sinus massage as a diagnostic and therapeutic tool for atrial flutter-fibrillation, 1998). Even if a coincidental conversion of AF into sinus rhythm could not be excluded, it is worthwhile to try CSM in every patient presenting with AF prior to other interventions to restore sinus rhythm.
Massage of the carotid sinus is contraindicated in patients with diseased carotid arteries because of the risk of cerebrovascular accidents; in rare instances, carotid sinus massage may initiate ventricular tachycardia.
The carotid sinus reflex should be considered an important test of vagal hypersensitivity (The cardioinhibitory carotid sinus reflex: Its importance as a vagocardiosensitivity test, 1963) and it is used to decrease high heart frequencies.