
DEFINITION
A syndrome of congenital facial paralysis, frequently associated with abducens palsy and other congenital abnormalities including lingual palsy, clubfeet, brachial disorders, cognitive deficits, and pectoral muscle defects. Pathologic findings are variable and include brain stem nuclear aplasia, facial nerve aplasia, and facial muscle aplasia, consistent with a multifactorial etiology. (Adams et al., Principles of Neurology, 6th ed, p1020)
EPIDEMIOLOGY
The exact incidence of Möbius syndrome is unknown. Researchers estimate that the condition affects 1 in 50.000 to 1 in 500.000 newborns. It affects boys and girls equally, and there appears to be, in some cases, an increased risk of transmitting the disorder from an affected parent to a child. Although no prenatal test for Moebius Syndrome is currently available, individuals may benefit from genetic counseling.
SYMPTOMS
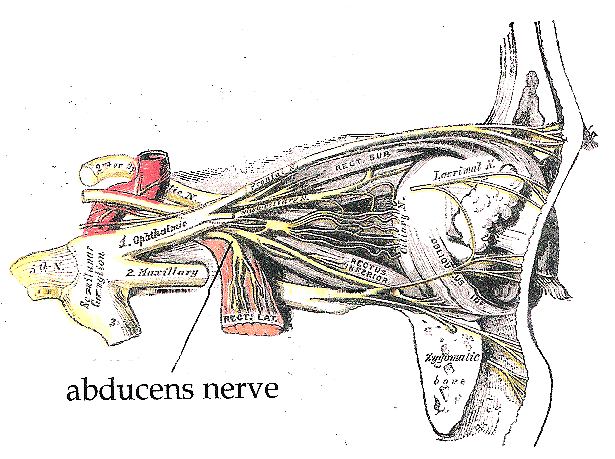
Due to a paralysis of the abducent and facial nerves, affected individuals can not smile, frown or raise their eyebrows; the inability to initiate facial movement may cause onlookers to believe that patients have no emotions, which can lead to social isolation (Self-perception of children and adolescents with Möbius sequence, 2011). The muscle weakness also causes problems with feeding, that become apparent in early infancy. In some individuals other cranial nerves may be involved and additional physical differences may be present. Other common symptoms are:
- Ocular motor: straight eyes, exoforia, esotropia with no horizontal movements and preserved vertical movements, total ophtalmoplegia, cocontraction of horizontal recti (decreased numbers of muscle fibres have been reported). In some patients eyelashes turn inward, causing problem with eye irritation. Irritation, corneal dryness and even corneal erosion can occur because of incomplete lid closure and difficulty blinking.
- Orofacial: hypoplasia of the tongue, bifid uvula, cleft lip, cleft palate, micrognathia, microstomia, external ear defects. An obvious consequence of this spectrum is difficulties in speech , expecially in bilabial sounds (B, M and P), pronunciation of which requires the lips to meet, and other consonant sounds such as F and V, which require the lower lip to meet the upper front teeth. Also problems in feeding are possible, like inability to suck or eating solid food. Caries are frequent, due to enamel hypoplasia and also to difficulty (in children) in removing food from their teeth and buccal spaces with their tongues during and after eating.

- Muscoloskeletal: syndactyly, brachydactyly, absent or supranumerary digits, arthrogryposis multiplex congenital, talipes.
- Miscellaneous: mental retardation, congenital heart defects, absent sternal head of the pectoralis major, degree of autism in 30 to 40% of children with Moebius syndrome (Autistic behaviour in Moebius syndrome, 1989), rib defects, Klippel-Feil anomaly, neuroradiologic cerebellar hypoplasia, hypogonadotropic, hypogonadism with or without anosmia.
PATHOGENESIS
Although most cases of Moebius syndrome are sporadic (i.e. they occur in people with no history of the disorder in their family) it's believed that the condition probably result from a combination of enviromental and genetic factors . Researchers have not identified any specific genes related to this condition; however, the disorder appears to be associated with changes in particular regions of chromosomes 3, 10 or 13 in some families: Slee et al. (1991) observed deletion of 13q12.2 in a 2.5-year-old girl with Moebius syndrome.
Ziter et al. (1977) observed congenital facial diplegia and flexion finger contractures in 7 members of 3 generations of a family. Each affected member showed an identical chromosome abnormality, reciprocal translocation between chromosomes 1p34 and 13q13. Unaffected family members had normal karyotypes. Both observations suggested that a gene responsible for Moebius syndrome is located in region 13q12.2-q13. Several modes of inheritance have been proposed, including X-linked recessive and autosomal dominant and recessive.
Affected members of the family of Krueger and Friedrich (1963) occurred in 3 generations, consistent with autosomal dominant inheritance.
Legum et al. (1981) reported 3 unrelated families with Moebius syndrome. One family was consistent with autosomal dominant inheritance, another family was consanguineous and consistent with autosomal recessive inheritance, and the third was a sporadic case with no family history. All affected patients had paresis of the facial and abducens nerves, with variable involvement of the other cranial nerves.
Baraitser (1977) stated that when myopathies have been excluded, the familial recurrence risk in the Moebius syndrome is no higher than 1 in 50.
Journel et al. (1989) described Moebius syndrome in 2 brothers and a male first cousin who were sons of sisters, thus suggesting X-linked recessive inheritance. The 2 brothers also had hypoplasia of the thumbs and absence of the big toes.
MacDermot et al. (1991) urged that the term 'Moebius syndrome' be restricted to cases with congenital VI and VII nerve paralysis with skeletal defects. They estimated a low familial recurrence risk, at about 2%. In their review, no recurrence was noted in 31 cases with cranial nerve palsies associated with oral abnormalities and limb defects. The features in an index case that may indicate a higher risk of recurrence are the absence of skeletal defects, isolated facial palsy, deafness, ophthalmoplegia, and digital contractures. As an example of the latter category, MacDermot et al. (1991) described mother and son with fifth, sixth, seventh, and bulbar cranial nerve paralysis who had 2 similarly affected relatives: the mother's maternal aunt and her son.
Graziadio et al. (2010) reported a mother and son with Moebius syndrome and skeletal anomalies. In infancy, the son was found to have a left facial palsy manifest as asymmetric crying facies, difficulty closing the eyes, and motility restriction of the left eye in all directions. He also had bilateral restriction of the hips and knees and clubfeet. Radiographic studies showed right coxa vara, left hip luxation, and osteopenia. At age 1 year, he had an expressionless face, sparse hair, high forehead, bitemporal narrowing, a broad but depressed nasal bridge, and strabismus. Other features included dimples in the elbows, short and tapering fingers, and sacral dimple. He had several surgeries to correct the lower limb skeletal anomalies. His 34-year-old mother had an expressionless face, strabismus, miotic pupils, bilateral facial palsy, osteopenia, hypoplasia of the iliac bones, coxa valga, small deformities of the left tibia and fibula, and clubfeet.
Anyhow, the most accepted cause of Moebius syndrome is vascular disruption, with a consequent temporary loss of bloodflow to the brainstem, that involves in brainstem calcification (Brainstem calcification in Möbius syndrome, 2004). An indisputed cause is environmental insults, expecially the use of drugs and medicine during pregnancy.

Misoprostol is the most extensively studied drug associated with the disease, followed by Thalidomide, Alcohol, Benzodiazepines and Ergotamines. Misoprostol is used to induce abortions in Brazil and Argentina as well as in the United States: abortions performed in this way are successful 90% of the time, while 10% of the time the pregnancy continues. Studies show that the use of misoprostol increases the risk of developing Moebius syndrome by a factor of 30 (Use of misoprostol during pregnancy and Möbius syndrome in infants, 1998). Also the use of Cocaine has been implicated in Moebius syndrome (Möbius syndrome in infant exposed to cocaine in utero, 1993).
Towfighi et al. (1979) proposed four recognized categories of Moebius syndrome:
- Group I, characterized by small or absent brain stem nuclei that control the cranial nerves;
- Group II, characterized by loss and degeneration of neurons in the facial peripheral nerve;
- Group III, characterized by loss and degeneration of neurons and other brain cells, microscopic areas of damage, and hardened tissue in the brainstem nuclei;
- Group IV, characterized by muscular symptoms in spite of a lack of lesions in the cranial nerve.

THERAPY
According to the National Institute of Neurological Disorders and Strokes (2007), there is no specific course of treatment for Moebius syndrome. Treatment is supportive, and in accordance with symptoms. Infants may require feeding tubes or special bottles to maintain sufficient nutrition (Haberman feeder).

Surgery may correct crossed eyes and improve limb and jaw deformities. Physical and speech terapy often improves motor skills and coordination, and leads to better control of speaking and eating abilities. (Brain plasticity in Möbius syndrome after unilateral muscle transfer: case report and review of the literature, 2012). Plastic reconstructive surgery may be beneficial in some individuals: a portion of the gracilis muscle in the thingh with its attached blood supply is transplanted to the face. The motor nerve (trigeminal) to the masseter muscle is used to innervate the gracilis muscles. Incision are made in the groin for removal of the gracilis and near the ears and hairline for transplanation to the face. In addition to facilitating facial animation with the ability to smile, the surgery provides lower lip support and improvement in drooling, drinking, speech and dental protection (Facial animation in children with Mobius syndrome after segmental gracilis muscle transplant, 2000).
Andrea Maccagno