MELAS is the acronym for Mitochondrial Encephalomyopathy, Lactic Acidosis, Stroke-like episodes. Patients with this syndrome have stroke-like events, acute in onset and associated with fever. This could be often confused with normal stroke episodes, but the brain vascular lesions are different in location.
These crisis are associated with migraine, vomit, often ischaemic-like episodes, hemiparesis and hemianopsia. They often occur in patients with cronical symptoms such as muscular deficiency, deafness, diabetes, cardiomyopathy, learning difficulties and memory ones.
The onset of this illness is due to point or microdeletion mutations in mitochondrial DNA and as all mithocondrial deseases, the transmission is inherited via the ovum and hence always from the mother.
Mitochondrial defect easily induce cardiomyopathy that may produce tipical cardioembolic strokes.
Anyway, the mitochondrial presentation and morphology are heterogeneous.

Epidemology
Males and females are equally affected. The prevalence is unknown, but the gene mutation (3243A>G) in the code for the Leu tRNA has a prevalence of 1/6250. This mutation is responsable of about the 80% of the cases.
MELAS is included in the register of rare diseas.
Symptoms
Patient’s history:
* Psychiatric problems
* Cognitive deficits
* Seizures
* Hearing loss
* Diabetes
* History of migraine with vomiting
The cerebral lesions favor the posterior regions of the hemispheres, with hemianopia and cortical blindness appearing more frequently than hemiparesis.
The stroke-like episodes are often followed by a complete recovery, but sometimes a progressive encephalopathy and other mental deficits hold over.
Furthermore, phisically, the patient have other symptoms such as muscle weakness, aphasia, cortical blindness, ataxia, tremor, hemianopia and psychiatric problems as dementia, psychosis and personality disorders.
Diagnosis
There are different types of examinations which could be done. The diagnosis is not very simple beacause MELAS is a multifactorial disease that is often misdiagnosed.
Lactic acid and pyruvate may be used as screening tests; high lactate could be exspecially found in cerebrospinal fluid, lactate and pyruvate in arterial blood.
Lactate and pyruvate may increase substantially with exercise.
The laboratory can also do a mitochondrial DNA analysis (notice that mitochondrial DNA is more susceptible than nuclear DNA).
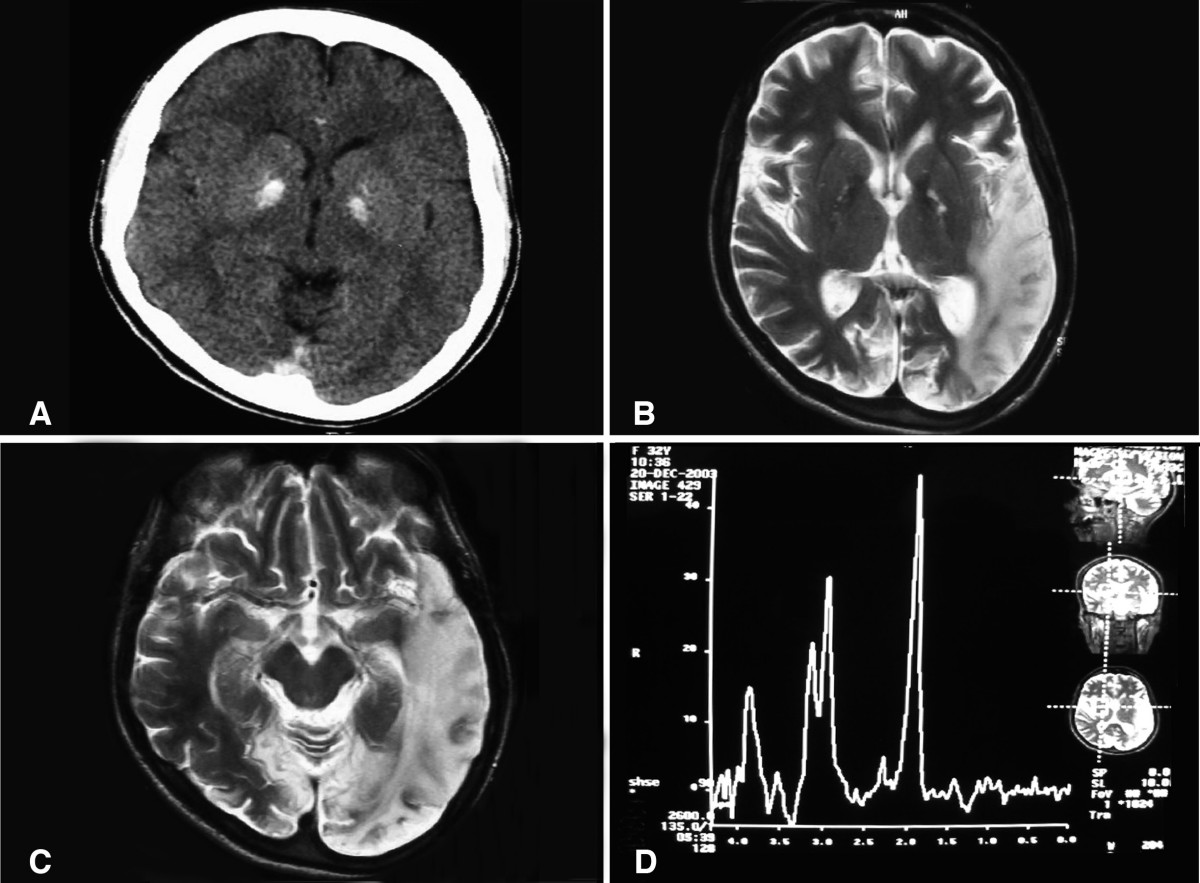
The CT scanning could find areas of stroke and basal ganglia calcification, that could be indentified also by a RMI.
Muscle biopsy demonstrates ragged red fibers on modified Gomori trichrome stain in at least 85% of cases, reflecting the proliferation of abnormal mitochondrias under the sarcolemma.
Pathologic examination of brain tissues demonstrates multiple cortical and subjacent white matter ischemic regions, spongiform degeneration of cortex, and calcium deposition in capillary walls of the globus pallidus.
Endothelial and smooth muscle cells of pial arterioles and small arteries exhibit increased numbers of structurally abnormal mitochondria, and capillary lumens are narrowed due to endothelial hypertrophy.
Elettroencephalography is very useful, exspecially in patients with seizures, because they occasionally have intractable status epilepticus as a terminal condition.
Compute Tomogaphy brain scan showing bilateral basal ganglia calcification.
Etiology
MELAS is a mitochondrial genetic disease. The main point of mutation (founded in the 80% of the affected) is the nucleotide position 3243 in Leucina tRNA. Anyway, there are 30 points of mutation associated with MELAS.
The stroke-like episodes seem to be associated with a defect in neuronal oxidative metabolism, where could exist a default in the electron-transport chain of the mitochondria, exspecially localized on the first(NADH dehydrogenase) and fourth complez of the chain, with a decrease of ATP production, leading to neuronal death. However, perfusion may be normal.
Another hypothesis suggested that the abnormal mitochondria caused a damaged autoregulation in endothelial and smooth muscle cells of blood vessels, where an anomalous nitric oxide metabolism persists.
The imaging techniques have shown that MELAS brain lesions are different from typical stroke ones and to be more precise, they are associated with increased blood flow, hyperemia, and vasogenic edema, rather than focal ischemia.
The Magnetic Resonance (MR) can show lactic acidosis increase.
There are also several case reports which associate MELAS with exposition to a drug used in migrain and mental illness, the Valproic acid. This drug may exacerbate the symptoms of MELAS.
Mutation of the tRNA Leu
p=. 
Natural history of MELAS associated with mitochondrial DNA m.3243A>G genotype. 2011
"Pathophysiology of the MELAS 3243 transition mutation. 1997":
http://www.ncbi.nlm.nih.gov/pubmed/9341162
Therapy
A number of experimental drugs, as coenzyme Q10, idebenone, dichloroacetate, cytochrome c, L-carnitine, L-arginine, and various B vitamins have been tried in MELAS patients, but the lack of long-term follow-up and the natural history of remission of lesions, however, hamper accurate evaluation of these drugs.
Coenzyme Q10 has some positive effects in patients, probably due to the increase in production of ATP at the inner mitochondrial membrane. In alternative to coenzyme Q10, it could be used Idebenone (an analogue of the coenzyme).
Dichloracetate is used to control acute symptoms of stroke-like episodes that often occur in patients with MELAS. His benfits are probably related to his effect of reduction of blood and brain lactate. However, randomized studies show no differences between dichloroacetate-treated patients and placebo-treated patients.
An important role is also due to repeated injections of cardiochrome that seems to reduce stroke-like episodes frequency. Cardiochrome is a combination of cytochrome c vitamins B-1 B-2, that increase the effectiveness of the electron transport chain of the inner mitochondrial membrane.
L- Arginine, used in a 15 MELAS patients cross section has been given some benfits, probably dued to the vasodilatation this amino acid induces.
It has been proved that Valproic acid, an atiepilectic drug, can’t be used in MELAS treatment, because of his detrimental effect on mitochondrias, that exacerbates seizures and stroke-like events.
If psychosis is present, the patient may benefit from psychiatric consultation.
Prognosis
Death in patients with MELAS is usually the result of cardiac failure, pulmonary embolus, or renal failure. Epileptic episodes can occasionally be fatal;
The tipical course of MELAS is characterized by neurological remissions and relapses, associated with progressive neuro-cognitive deficits. Most of the patients died by the fourth decade for medical complications, but it’s known that some patients even arrived in the sixth decade.
Marco Marzolla e Alessandro Strumia