DEFINITION
Polycystic ovary syndrome (PCOS) is a complex and heterogeneous disorder affecting approximately 7 per cent of women of reproductive age.
The etiology of polycystic ovary syndrome is unknown. What is certain is that the syndrome is a major cause of anovulatory infertility.
SYMPTOMPS
The PCOS is characterized primarily by chronic anovulation, hyperandrogenemia, altered LH: FSH ratio (>2/3:1) and polycystic ovaries.
In the majority of cases PCOS is diagnosed because amenorrhea, obesity or overweight, acne or hirsutism occur.
The most common characteristic is the menstrual abnormality: menstrual intervals can be longer than 35 days and there are fewer than eight menstrual cycles a year.
The elevated levels of male hormones result in excess facial and body hair (hirsutism) and adult or severe adolescent acne.


In these women the ovaries appear polycystic so characterized by an increase in antral follicles and ovarian stroma as well as by theca cell hyperplasia and ovarian cortical thickening.


COMPLICATIONS
Having polycystic ovary syndrome, especially if also obesity is a factor, makes the following conditions more likely:
• type 2 diabetes;
• high blood pressure;
• insulin resistance;
• elevated levels of C-reactive protein, a cardiovascular disease marker;
• nonalcoholic steatohepatitis;
• gestational diabetes or pregnancy-induced high blood pressure;
• cancer of the uterine lining, caused by exposure to continuous high levels of estrogen;
• metabolic syndrome, a cluster of signs and symptoms that indicate a significantly increased risk of cardiovascular disease.
(Diseases and Conditions: Polycystic ovary syndrome (PCOS), Mayo Clinic)
Therefore, expecially if the obesity (or the overweight) increases the condition, PCOS becomes a factor and a part of an heterogeneous disorder called "metabolic syndrome", in which the metabolism of carbohydrates and the pathway of insulin play a very significant role.
A FOCUS ON THE METABOLIC SYNDROME
Metabolic syndrome is a disorder of energy utilization and storage, diagnosed by a co-occurrence of three out of five of the following medical conditions: abdominal obesity, elevated blood pressure, elevated plasma glucose, high serum triglycerides, and low high-density cholesterol (HDL) levels. Metabolic syndrome increases the risk of developing cardiovascular disease, particularly heart failure, and diabetes. (Metabolic syndrome, wiki)

PCOS AND INSULINE RESISTANCE
The association between a disorder of carbohydrate metabolism and hyperandrogenism was first described in 1921 by Achard and Thers and was called "the diabetes of bearded women" (Andrea Dunaif, Insulin Resistance and the Polycystic Ovary Syndrome: Mechanism and Implications for Pathogenesis , 1997)
Insulin resistance is defined clinically as the inability of a known quantity of exogenous or endogenous insulin to increase glucose uptake and utilization in an individual as much as it does in a normal population. (Prevalence and clinical profile of insulin resistance in young women of poly cystic ovary syndrome: A study from Pakistan, 2013)
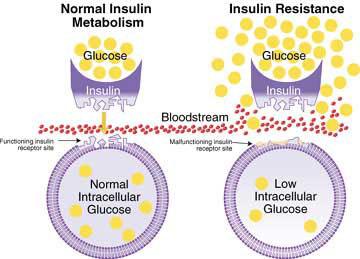
Insuline resistance is very common and plays a central pathogenic role in PCOS, it is present in approximately 50-70 per cent of these women. In the last years several studies have been conducted to understand the mechanisms contributing to the state of insulin resistance and insulin-induced hyperandrogenemia in PCOS.
The studies about insulin signaling pathways in different responsive tissues - such as adipose tissues, skeletal muscles, adipose tissues, fibroblasts as well as ovaries - suggest a post receptor signaling defect: metabolic action of insulin is compromised but not the steroidogenic and mitogenic actions. (Molecular & genetic factors contributing to insulin resistance in polycystic ovary syndrome, 2010)
In PCOS there is a kind of paradox: ovary remains sensitive to insulin action to produce androgens in spite of systemic insulin resistant state; in fact classical target organs of insulin remain resistant to its metabolic activity. IR progresses towards the development of compensatory hyperinsulinemia, and hyperinsulinemia implies hyperandrogenemia.

For these reasons in the women affected by PCOS high androgen levels lead to menstrual disturbances, development of ovarian cysts and hirsutism, all clear symtomps typical of the disorder.
IR also increases the risk for development of glucose intolerance, type 2 diabetes mellitus, hypertension, dyslipidaemia and cardiovascular abnormalities in these women.

PCOS, IR AND OBESITY
Women with PCOS are frequently obese and this condition is an important component of IR.
Why?
Adipocytes are not simply a storage depot: they are also endocrine organs, with multiple metabolic roles. The enlarged adipocytes of obese individuals recruit macrophages and promote inflammation and the release of a range of factors that predispose toward insulin resistance.
The adipocyte hormones leptin and adiponectin activate the AMP-activated protein kinase (AMPK) in muscle and other tissues, a pathway that increases fat oxidation and glucose transport.
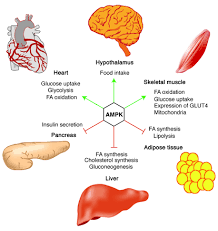
Also physical exercise activates the AMPK and, importantly, the same pathway is activated by the antidiabetic agents such as thiazolidinediones and metformin, used in the therapy of PCOS.
Leptin is a peptide hormone secreted by adipose tissue in proportion to its mass. This hormone circulates in blood and acts on receptors in the hypothalamus of the brain, where it inhibits appetite counteracting the effects of neuropeptide Y (that on the contrary stimulates the appetite) and supporting the synthesis of α-MSH, an appetite suppressant.
When fat mass increases, leptin blood level increases, suppressing appetite until weight is lost.
However obese individuals generally exhibit an unusually high circulating concentration of leptin : they are resistant to the effects of leptin. The high concentrations of leptin from the enlarged adipocytes drives leptin desensitization, so the body does not adequately receive the satiety feeling subsequent to eating.
Also adiponectin is synthetised by adipocytes and its plasma concentration falls with increasing obesity. Reduced adiponectin concentrations correlate with insulin resistance, hyperinsulinemia and hypertrophy of the adipocytes. In addition, several polymorphisms of the adiponectin gene (APM1, mapped to chromosome 3q27) have been identified that are associated with reduced plasma adiponectin concentration and that increase the risk of type 2 diabetes, insulin resistance, and of the metabolic syndrome.+Adiponectin acts as an insuline-sensitizing agent+ on the liver and has an anti-inflammatory function, so the opposite function of TNF-α and Interleukin-6 (IL-6).
Finally adipose tissue in obese persons shows higher expression of pro-inflammatory proteins, including TNF-α and IL-6.
TNF-α increases systemic insulin resistance by promoting the release of fatty acids from adipose tissue.
In the same condition IL-6(whose concentration correlates with insulin resistance) increases lipolysis and fat oxidation.
(Obesity and the role of adipose tissue in inflammation and metabolism, 2006)

Moreover, there is a relationship between iron deficiency and obesity: in fact the chronic low-grade inflammation that characterizes obesity enhances hepcidin production, the principal regulator of iron availability. Interleukin-6 and leptin secreted by adipose tissue trigger hepcidin production. (The role of adipocytes in the modulation of iron metabolism in obesity.)
Then, hepcidin inhibits iron transport across the gut mucosa reducing iron absorption and also inhibits transport of iron out of macrophages (site of iron storage and transport). So, in states of high hepcidin levels (including inflammatory states such as the obesity), serum iron levels fall. (Hepcidin, wiki)
A considerable iron deficiency ends up paralysing mechanisms and pathways that need iron, first of all the mitochondrial elecron transport chain that drives ATP synthesis. In particular is known that the cytochrome complex, or cyt c is a small heme protein associated with the inner mithocondrial membrane that transfers electrons between Complexes III (Coenzyme Q - Cyt C reductase) and IV (Cyt C oxidase) through the passage from the ferric iron (oxidized form) to ferrous iron (reduced form). If the iron level is very low the cyt c and all the chain may not to operate well and the muscle prefer not to oxidize energetic substrates, principally the glucose. In this way it may become not responsive to insuline (because it doesn’t manage to use glucose) and aids the condition of insuline resistance.

THERAPY
Because of the several implications and disorders of the PCOS the treatment must act at different levels:
- Regulating the menstrual cycle and treating body and face hair. If the patient doesn’t want to become pregnant a combination estrogen/progestin contraceptives are the better treatment and will also relieve hyperandrogenism without affecting insulin resistance. Anti-androgen therapy, such as spironolactone (that blocks the effects of androgens on the skin) can be added for further treatment of hirsutism.
- Aiding the ovulation, if the woman with PCOS wants to become pregnant instead.
- Improving the insuline resistance.
About the last two points it is funded by now that the two major pharmacological approaches to the treatment of diabetes are also an efficient therapy of PCOS.
These are the insulin sensitizers: the biguanide metformin and the thiazolidinediones troglitazone, pioglitazone, and rosiglitazone. These agents improve not only glucose control, but also the reproductive abnormalities associated with PCOS.
Metformin modestly increases menstrual regularity and ovulation and decreases weight and hyperandrogenism. It improves insulin resistance, increases peripheral glucose uptake and decreases hepatic glucose production.
New agents under investigation for use in PCOS include pramlintide and D-chiro-inositol. Pramlintide is an analog of amylin, a β-cell hormone that is normally co-secreted with insulin; it complements the effects of insulin in postprandial glucose control, in part by suppressing glucagon secretion. D-chiro-inositol is an insulin sensitizer that has preliminarily been shown to increase ovulation in PCOS.
If drugs are not enough to avoid a pregnancy, gonadotropins so follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are administered by injection. Moreover an outpatient surgery called “laparoscopic ovarian drilling” is an option for few candidate women with PCOS. The surgeon makes a small incision in the abdomen, inserts a tube attached to a camera (laparoscope) and uses electrical or laser energy to burn holes in follicles on the surface of the ovaries. The aim of the surgery is to induce ovulation.

THE BEST THERAPY
However, the safest and cheapest therapy that has shown benefit both in diabetes and PCOS is weight loss by lifestyle modification.
Several studies have revealed that even modest weight loss (10–20%) improves all symptoms of PCOS in obese patients: acne, hirsutism, and menstrual irregularities.
The improvements are likely a result of the reductions in insulin levels, insulin resistance, dyslipidaemia and hypertension (all factors of the metabolic syndrome). Then weight loss can reduce androgen levels, and may restore ovulation.
It is useful to pay attention to dietary composition: increasing fiber intake (because fiber slows nutrient absorption after meals and reduces insulin secretion), reducing both carbohydrates and the total calories intake.
Finally, as a lifestyle modification, physical exercise helps sustain weight loss, but it also has other benefits.
 Exercise can increase glucose disposal and muscle sensitivity to insulin. In PCOS, women who self-reported 8 hours of sports activities per week had improvement in acne and menstrual irregularities.
Exercise can increase glucose disposal and muscle sensitivity to insulin. In PCOS, women who self-reported 8 hours of sports activities per week had improvement in acne and menstrual irregularities.
Exercise as the primary intervention without attendant weight loss (< 5% weight loss) improved insulin sensitivity and testosterone index and induced ovulation in 9 of 18 obese PCOS patients.
(Polycystic Ovary Syndrome and the Metabolic Syndrome, 2003)
The key enzyme of all the therapies is certainly the 5' AMP-activated protein kinase or AMPK that plays a central role in cellular energy homeostasis.
It is expressed in various tissues, including the liver, the brain, and the skeletal muscle. The functions of AMPK are: stimulation of hepatic fatty acid oxidation, inhibition of cholesterol synthesis, lipogenesis, and triglyceride synthesis, inhibition of adipocyte lipolysis, stimulation of skeletal muscle fatty acid oxidation and muscle glucose uptake, and modulation of insulin secretion by pancreatic beta-cells.
Then, clearly the AMPK pathway involves all the targets implied in the more difficult complications of PCOS, so the metabolic syndrome and the insuline resistance.
Both the drug therapy, first of all the metformin, and the muscle contraction close in the activation of this enzyme, that is also the target of leptin and adiponectin.

CONCLUSION
The PCOS is a very heterogeneous disorder that needs an early diagnosis to avoid the regression in the worse manifestations, such as the diseases related with the carbohydrates metabolism and the insulin resistance.
Either way there are valid solutions and treatments for both women who want to plan a pregnancy, and not.
Anyway, the most prudent and natural approach to this disorder corresponds to adjust the lifestyle with a correct and adapt diet and above all an healthy and moderate physical exercise.