Rickets is defective mineralization of bones before epiphyseal closure
in immature mammals due to deficiency or impaired metabolism of vitamin D , phosphorus or calcium, potentially leading to fractures and deformity. Rickets is among the most frequent childhood disease in many developing countries. The predominant cause is a vitamin D deficiency, but lack of adequate calcium in the diet may also lead to rickets (cases of severe diarrhea and vomiting may be the cause of the deficiency). Although it can occur in adults, the majority of cases occur in children suffering from severe malnutrition, usually resulting from famine or starvation during the early stages of childhood.
Signs and symptoms
The clinical presentation of nutritional rickets depends on the age of the child, it includes soft skull bone, called craniotabes; hypocalcaemic convulsions; typical bone deformities like deformation of the weight-bearing limbs; swelling of the wrist, knee or ankle; swelling of the costochondral junction of the ribs, called rachitic rosary or the deformity of the soft rib cage due to pulling of the diaphragm, called Harrison's sulcus. Furthermore, muscular hypotonia or delayed motor development may occur.
The biochemical findings of nutritional rickets include a normal or decreased blood level of calcium, a normal, decreased or increased blood level of phosphate as well as elevated blood levels of alkaline phosphatase, parathyroid hormone or both. In vitamin D-deficiency rickets 25-hydroxyvitamin D blood levels are decreased.
Radiologically, there is an irregular metaphyseal outline like cupping, widening or fraying due to diminished calcification of the growth plate. In younger children the radiological changes can best be visualised in the wrist, in older children the area above and below the knee is most useful.(Interventions for the prevention of nutritional rickets in term born children. ; Rickets and vitamin D deficiency in children and adolescents.:)


Diagnosis
Rickets may be diagnosed with the help of:
Blood tests
Serum calcium may show low levels of calcium, serum phosphorus may be low, and serum alkaline phosphatase may be high from bones or changes in the shape or structure ofthe bones. This can show enlarged limbs and joints.
Bone biopsy is rarely performed but will confirm rickets.
Pathogenesis: Vitamin D and calcium
In general, nutritional rickets is the result of either calcium or vitamin D deficiency, or both.
The exposure of the skin to ultraviolet light (wavelengths from 290 to 315 nm, called UV-B) is crucial for the beginning of the endogenous syntheses of vitamin D. Provitamin D 3 (7-dehydrocholesterol), stored in the skin, is photolysed by the absorbed energy of UV-B to previtamin D 3 . Previtamin D 3 converts to vitamin D 3 (cholecalciferol) rapidly. Thus, low UV-B irradiation due to northern or southern latitude, high air pollution, short outdoors exposure time, veiling of the skin, the use of sunscreens or high amounts of the skin pigment melanin lower the production of vitamin D 3 . As vitamin D 3 is synthesised due to sunlight exposure, it is not a vitamin in the strict sense of definition.
Exogenous sources of vitamin D provide vitamin D 2 (ergocalciferol) and vitamin D 3 . Very few foods contain a reasonable amount of vitamin D. Human breast milk has only a low concentration of vitamin D, which is an important factor for infants being solely breast fed for a long time.
Vitamin D, which denotes both vitamin D 2 and vitamin D 3 , is hydroxylated in the liver to 25-hydroxyvitamin D (calcidiol). A further hydroxylation, mainly in the kidneys, leads to 1,25-dihydroxyvitamin D (calcitriol), the final active form of vitamin D.
1,25-dihydroxyvitamin D acts via the vitamin D receptor (VDR), an intracellular protein which belongs to the steroid-hormone-thyroid hormone-retinoic acid receptor gene superfamily. Conflicting data exist for the role of polymorphisms of VDR for the pathogenesis of rickets.
The target of VDR is the vitamin D response element regulating gene transcription which evokes in the intestine the synthesis of proteins necessary for the transfer of calcium from the intestinal lumen to the capillaries. It is assumed that only ten percent of the calcium entry is vitamin D independent. The availability of calcium is lowered by complexation with oxalate or phytate. Inadequate low intake of calcium leads to inactivation of calcidiol.
A high-fibre diet results in degradation of calcitriol, as does elevated parathyroid hormone resulting from hypocalcaemia.
In state of dietary calcium deficiency, vitamin D also interacts with VDR in bone tissue. The thereby induced maturation of osteoclasts leads to dissolving of bone tissue and thus, release of calcium. It is not clear whether there is a direct effect of vitamin D on bone formation, too.
There are many other actions of vitamin D besides the regulation of calcium homeostasis, for example regulation of cell growth and apoptosis being associated with several forms of cancer. Furthermore, the modulation of immune reactions is associated with autoimmune diseases like type 1 diabetes mellitus or multiple sclerosis. There are influences on the functions of muscles and the nervous system, too. (Interventions for the prevention of nutritional rickets in term born children ; Mechanisms of intestinal calcium absorption ; Vitamin D)

Epidemiology
Nutritional rickets has been described as a public health problem in several countries over the past 30 to 40 years. Affected countries and regions include the United Kingdom, the United States, Greece, Turkey, the Middle East, China, Mongolia, Tibet, Ethiopia, Nigeria, Somalia, and others. The peak age for the development of rickets is between 6 and 18 months;however, it appears that in certain communities adolescence is anotherperiod during which the incidence of rickets and osteomalacia increases.(Rickets and vitamin D deficiency in children and adolescents)
Treatement and Prevention
Treatment involves increasing dietary intake of calcium, phosphates and vitamin D. Exposure to ultraviolet B light (most easily obtained when the sun is highest in the sky), cod liver oil , halibut-liver oil, and viosterol are all sources of vitamin D.
A sufficient amount of ultraviolet B light in sunlight each day and adequate supplies of calcium and phosphorus in the diet can prevent rickets. Darker-skinned people need to be exposed longer to the ultraviolet rays . The replacement of vitamin D has been proven to correct rickets using these methods of ultraviolet light therapy and medicine.
Recommendations are for 400 international units (IU) of vitamin D a day for infants and children. Children who do not get adequate amounts of vitamin D are at increased risk of rickets. Vitamin D is essential for allowing the body to uptake calcium for use in proper bone calcification and maintenance.
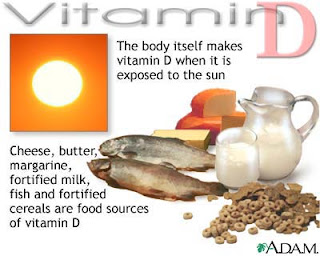
Sufficient vitamin D levels can also be achieved through dietary supplementation and/or exposure to sunlight. Vitamin D3 (cholecalciferol) is the preferred form since it is more readily absorbed than vitamin D2. Most dermatologists recommend vitamin D supplementation as an alternative to unprotected ultraviolet exposure due to the increased risk of skin cancer associated with sun exposure. Endogenous production with full body exposure to sunlight is approximately 250 µg (10,000 IU) per day.