Definition
Eosinophilic Gastroenteritis (EGE) is a rare and heterogeneous gastrointestinal disease characterised by eosinophilic infiltration in the gastrointestinal tract.
It can involve more than one layer and any part of the gastrointestinal tract, but the stomach and the proximal small bowel are the most common sites of involvement. Biliary obstruction is an unusual presentation of EGE and there are just few case reports of biliary involvement.
Eosinophilic gastroenteritis mimicking pancreatic cancer, 2002
Eosinophilic gastroenteritis causing pancreatitis and pancreaticobiliary ductal dilation, 2002
Clinical features depend on which layer and site are involved.
EGE is classified into three forms (mucosal, muscular and serosal) depending on the depth of involvement.
Epidemiology
Available data about the epidemiology of EGE are limited. Although it can affect all ages, the majority of cases occur in adults in the third to the fifth decades of life. It can affect both sexes although it seems to be more common in men.
An accurate epidemiological estimations for EGE doesn’t exist to date, but an incidence of approximately one case per 100,000 inhabitants has been traditionally proposed. The total number of patients described so far is less than four hundred.
An American electronic survey has recently estimated an overall prevalence of 28/100,000 for EGE.
Variation in prevalence, diagnostic criteria, and initial management options for eosinophilic gastrointestinal diseases in the United States, 2011
Eosinophilic Gastroenteritis. An Update, 2012
Pathogenesis
Limited research has been developed on the molecular basis of EGE. The pathophysiology of EGE is poorly known and due to its low prevalence, most of available information comes from individual case reports and short case series.
Increased production of interleukin-5 and activated eosinophilis has been demonstrate to be the rule and a vast proportion of patients shows peripheral eosinophilia
A part from EGE, eosinophils have been implicated in the pathogenesis of many disorder as well as allergic reaction, asthma , atopic dermatitis. As a part of host defence mechanism, eosinophilis are normally present in gastrointestinal mucosa, even if the finding in deeper tissue is typically pathologic.
A predominant aspect in EGE is the recruitment of eosinophilis in the tissue. Defining the mechanisms that control recruitment is fundamental to understanding the disease process. A lot of substances have chemotactic activity for eosinophils, including IL-5 and IL-3 , granulocyte-macrophage colony-stimulating factor (GM-CSF) and especially eotaxin, a chemokine espressed throughout the gastrointestinal tract. Eotaxin induces significant eosinophil transmigration in vitro and its effect depends predominantly on the activation of the plasminogen-plasmin system.
Eotaxin and eosinophil recruitment: implications for human disease, 2000
A pathological function for eotaxin and eosinophils in eosinophilic gastrointestinal inflammation, 2001
Eotaxin promotes eosinophil transmigration via the activation of the plasminogen-plasmin system, 2001
Some works also suggest that gastrointestinal eosinophils express the alpha4beta7integrin, which is responsible, in part, for eosinophilic homing.
LPAM (alpha 4 beta 7 integrin) is an important homing integrin on alloreactive T cells in the development of intestinal graft-versus-host disease, 2004
Gastrointestinal eosinophils, 2001
In summary, eosinophils are resident cells of the gastrointestinal immune system whose levels can be induced by antigen exposure under Th2 conditions, in a manner that is critically regulated by eotaxin and IL-5.
Interleukin-5 in eosinophilic gastroenteritis, 1992

Elevated total IgE , specific IgE to food antigens and eosinophilia characterize allergic eosinophilic gastroenteritis. Added to IL-5, other cytokines like IL-4 and gamma interferon regulate IgE synthesis and eosinophilopoiesis in vitro. These lymphokine present an imbalanced production in allergic EGE, consistent with the eosinophilia and elevated IgE that characterized this disease.
Evidence for an abnormal profile of interleukin-4 (IL-4), IL-5, and gamma-interferon (gamma-IFN) in peripheral blood T cells from patients with allergic eosinophilic gastroenteritis, 1994
Tissue Damage
Cytotoxic proteins contained in eosinophils cytoplasm granules are capable of causing cell damage. Secretory IgA has been demonstrated to be one of the most powerful stimulants for eosinophilic degranulation.
Major Basic Protein has direct toxic effects on various mammalian cells; in addition it can cause mast-cell degranulation which may augment the inflammatory response by releasing of proinflammatory cytokines.
Eosinophilic gastroenteritis: Current aspects on etiology, pathogenesis, diagnosis and treatment, 2002

Allergy-Food Hypersensitivity
EGE has been related to food allergies. Many patients indeed have history of atopic disorders such as eczema, asthma, drug allergies, hypersensitivity to food.
In some patients with the mucosal form, the disease reflects allergy to some components of the diet; these patients usually present a family history of atopy and elevated IgE serum levels. Diary products are often implicated in the causation of EGE. Foods that appear to be related include eggs, milk protein, beef, pork, gluten-flour products. Food allergy has been reported to be present in 50% of patients.
Unusual presentations of eosinophilic gastroenteritis: Case series and review of literature, 2009
Eosinophilic gastroenteritis: Current aspects on etiology, pathogenesis, diagnosis and treatment, 2002
Presentation of various atopic manifestations reinforce the idea that eosinophils accumulate in the stomach and small bowel in response to exposure to food or environmental antigens. In most EGE patients are also observed clinical and histological responses to therapies used in allergic disease and dietary modifications.
Eosinophilic Gastroenteritis. An Update, 2012
Symptoms and Signs
Signs and symptoms of EGE depend on the depth of bowel wall involvement. Symptoms include nausea, vomiting, diarrhea, abdominal pain, weight loss. Accompanying symptoms include eczema, asthma, rhinitis.
According to Klein (Eosinophilic gastroenteritis, 1970) proposal the disease can be classified into three different patterns :
- Mucosal form is the most common variety, characterized by mucosal and submucosal involvement that produce malabsorption with anemia and protein-loosing enteropathy. Symptoms include nausea, diarrhea, weight loss and abdominal pain
- Muscular form : the inflammation of muscle layers leading to digestive wall thickening and obstructive symptoms. The stomach and duodenum are the most affected segments
- Serosal form or eosinophilic ascitis : this form is relatively uncommon. Serosal involvement can produce painful peritonitis and ascites consisting of trasudate rich in eosinophils
Clinical presentation of EGE could be quite wide. There are case reports of patients with intestinal perforation; this complication usually requires surgical repair.
Peripheral blood eosinophilia is frequently being found and it is more frequent in patients with mucosal and serosal form.
Although EGE can involve the entire gastrointestinal tract, the esophagus and colon are uncommonly involved. However, esophageal involvement is now more frequently reported, especially in children and young adults. The stomach and duodenum have been proposed as the most frequently involved digestive organs, but these are also the most examined digestive segments by means of endoscopy, so it remains uncertain whether this represents a bias.
Small bowel involvement may present with abdominal pain, diarrhea or frank malabsorption and rarely bowel obstruction.
Unusual presentations of eosinophilic gastroenteritis: Case series and review of literature
Eosinophilic Gastroenteritis. An Update, 2012
Biliopancreatic involvement has been descrive; these patients present bile duct dilation, obstruction or jaundice, togheter with symptoms derived from gut inflammation.
Biliary tract disease: a rare manifestation of eosinophilic gastroenteritis, 2003
Recurrent acute pancreatitis due to eosinophilic gastroenteritis. Case report and literature review, 2006
Natural History of EGE
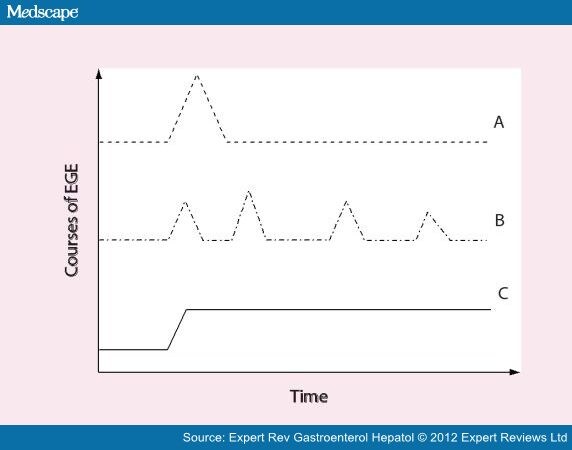
A recently published French study analyzed the data on initial clinical presentation and long-term outcomes of 43 adult patients with EGE who were followed for a period of 13 years. The authors described three different courses of disease progression : 42% had an initial flare of the disease without relapse; 37% of patients exhibited a recurrent pattern of disease (multiple flares that were separated by periods of full remission) and finally 21% of patients had a chronic disease with persistent symptoms.
Natural history of eosinophilic gastroenteritis, 2001
Diagnosis
Talley (Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues, 1990) suggested 3 diagnostic criteria :
- the presence of gastrointestinal symptoms
- eosinophilic infiltration in one or more areas of the gastrointestinal tract or peripheral eosinophilia
- no evidence of parasitic or extraintestinal disease
Peripheral eosinophilia may not be present in all patients; tissue eosinophilia may support the diagnosis even if it is a component of various other disorder.
In order to exclude a possible secondary cause of EGE, a detailed history of drug use should be obtained in all cases. A vast number of pharmaceutical agents can cause peripheral hypereosinophilia, such as Enalapril.
Enalapril-induced eosinophilic gastroenteritis, 2001
Endoscopy
The endoscopy appearance is nonspecific, with mucosal hyperemia and thickened gastric folds being the most common. Findings include areas of rough or nodular appearance, erosions, aphthae and ulcers, multiple erythematous lesions, loss of villi and incomplete strictures with ulcerated mucosa alternating with preserved areas.
In some cases, the endoscopic findings were normal.
Radiology
Radiological findings are unspecific in two thirds of patient. Double-contrast radiographies are usually normal, but in some cases they show thickened folds, irregular or serrated edges in the small intestine walls, nodular contrast defects or slow contrast progression indicative of gastrointestinal hypomotility.
Double-Contrast Upper Gastrointestinal Radiography: A Pattern Approach for Diseases of the Stomach, 2008
Pathologic findings
There are no standards for making the istologic diagnosis; the eosinophilic infiltration tends to affect specific layers of the gastric or intestinal wall and lesions are usually multiple and patchy. Eosinophilic infiltration may cause epithelial cell necrosis, pit or crypt abscesses, erosions, shallow ulcers, or villous atrophy. When the main site of eosinophilic infiltration is restricted to the mucosa, it tends to produce edema, lymphatic dilatation and intense sheet-like eosinophilic infiltrate. It is not uncommon to find eosinophilic infiltration of the gastric pits, of the duodenum with villous atrophy or the infiltration of the muscularis mucosa and extention into the submucosa with associated edema.
Eosinophilic gastroenteritis: Current aspects on etiology, pathogenesis, diagnosis and treatment, 2002
Treatment
Dietary treatment

Only a small number of patients enter remission with diet therapy alone, they represent a unique subpopulation of those with EGE.
The disease can appear before the age of 1 year and resolves after cow’s milk elimination from the diet, similar results have been reported for adult patients.
Eosinophilic gastroenteritis due to allergy to cow's milk, 2011
It is possible to achieve complete resolution of eosinophilic infiltration by exclusive feeding with an amino acid-based elemental diet. Once the remission is achieved, specific foods should be reintroduced progressively, identifying problem foods by the return of symptoms.
No agreement exists in the literature as to which allergic tests should be carried out un EGE patients.
Eosinophilic Gastroenteritis. An Update, 2012
Drug therapy
Corticosteroids have been the most widely used drugs for treating EGE in both children and adults. Prednisone has proven highly effective in the initial control of symptoms, eosinophilic tissue infiltration, blood hypereosinophilia and also for controlling ascitis. After 7-10 days of therapy the dose can frequently be tapered slowly over several weeks.
A few patients require continuous, long-term steroids to maintain remission.
Disease recurrence is more likely in those patients requiring treatment at the moment of diagnosis as compared with those who exhibit spontaneous remission. Patients with recurrent disease may also present a higher blood eosinophil count at diagnosis.
Also a stabilizer of mast cell membranes such as sodium cromolyn, ketotifen (an antihistamine), leukotriene inhibitor montelukast have been proposed, with mixed results.
Subserosal eosinophilic gastroenteritis treated efficaciously with sodium cromoglycate, 1997
Eosinophilic Gastroenteritis. An Update, 2012
Surgical treatment
Even after bowel resection , recurrence in another segment of the bowel is common. In the absence of obstructive symptoms, surgery should not be undertaken solely to confirm the diagnosis before a trial of corticosteroid therapy.
Repeated bowel resections for eosinophilic gastroenteritis with obstruction and perforation. Case report, 1990 Apr
Eosinophilic gastroenteritis: Current aspects on etiology, pathogenesis, diagnosis and treatment, 2002