more about this topic 

Medium-chain triglyceride ketogenic diet and epilepsy 2018 Fulltext
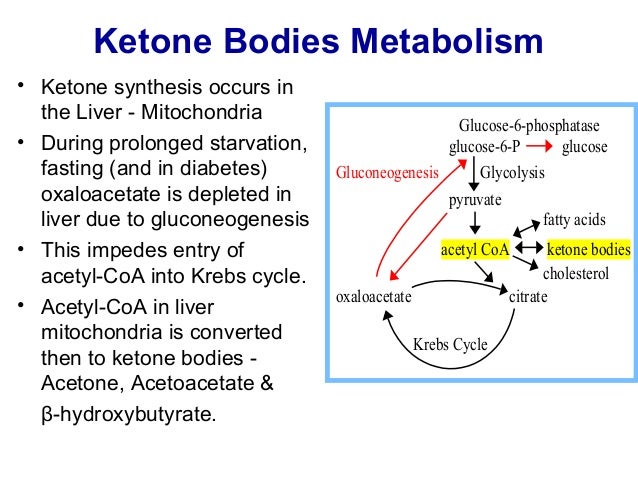
- High-fat, low-carbohydrate diets, known as ketogenic diets, have been used as a non-pharmacological treatment for refractory epilepsy. A key mechanism of this treatment is thought to be the generation of ketones, which provide brain cells (neurons and astrocytes) with an energy source that is more efficient than glucose, resulting in beneficial downstream metabolic changes, such as increasing adenosine levels, which might have effects on seizure control. However, some studies have challenged the central role of ketones because medium-chain fatty acids, which are part of a commonly used variation of the diet (the medium-chain triglyceride ketogenic diet), have been shown to directly inhibit AMPA receptors (glutamate receptors), and to change cell energetics through mitochondrial biogenesis. Through these mechanisms, medium-chain fatty acids rather than ketones are likely to block seizure onset and raise seizure threshold. The mechanisms underlying the ketogenic diet might also have roles in other disorders, such as preventing neurodegeneration in Alzheimer’s disease, the proliferation and spread of cancer, and insulin resistance in type 2 diabetes. Analysing medium-chain fatty acids in future ketogenic diet studies will provide further insights into their importance in modified forms of the diet. Moreover, the results of these studies could facilitate the development of new pharmacological and dietary therapies for epilepsy and other disorders.
 medium-chain fatty acids and ketogenic diet
medium-chain fatty acids and ketogenic diet
How Can a Ketogenic Diet Improve Motor Function? 2018
- A ketogenic diet (KD) is a normocaloric diet composed by high fat (80–90%), low carbohydrate, and low protein consumption that induces fasting-like effects. KD increases ketone body (KBs) production and its concentration in the blood, providing the brain an alternative energy supply that enhances oxidative mitochondrial metabolism. In addition to its profound impact on neuro-metabolism and bioenergetics, the neuroprotective effect of specific polyunsaturated fatty acids and KBs involves pleiotropic mechanisms, such as the modulation of neuronal membrane excitability, inflammation, or reactive oxygen species production. KD is a therapy that has been used for almost a century to treat medically intractable epilepsy and has been increasingly explored in a number of neurological diseases. Motor function has also been shown to be improved by KD and/or medium-chain triglyceride diets in rodent models of Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, and spinal cord injury. These studies have proposed that KD may induce a modification in synaptic morphology and function, involving ionic channels, glutamatergic transmission, or synaptic vesicular cycling machinery. However, little is understood about the molecular mechanisms underlying the impact of KD on motor function and the perspectives of its use to acquire the neuromuscular effects. The aim of this review is to explore the conditions through which KD might improve motor function. First, we will describe the main consequences of KD exposure in tissues involved in motor function. Second, we will report and discuss the relevance of KD in pre-clinical and clinical trials in the major diseases presenting motor dysfunction.
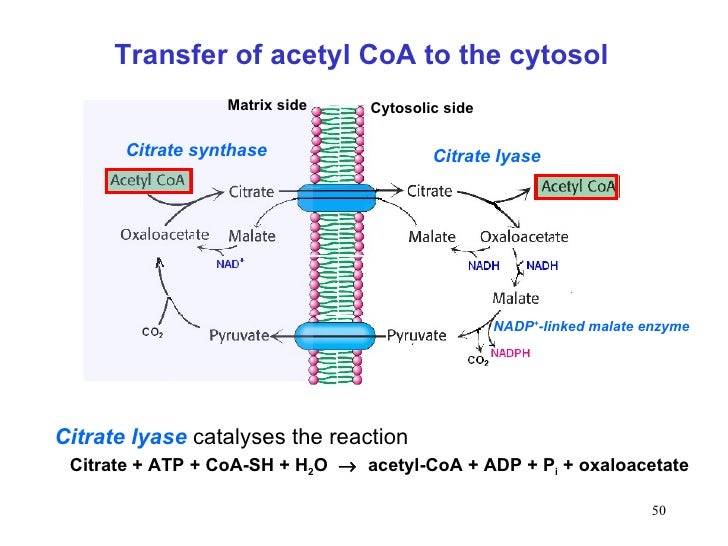

Roles of the PMCT and the CTP in supplying citrate to fuel hepatic fatty acid, triacylglycerol, and sterol biosyntheses