Origins and functions of the circadian rhythms and their participation in the metabolism.
Biological clocks are genetically encoded oscillators that allow organisms to anticipate changes in the light-dark environment that are tied to the rotation of the Earth.
These “clocks” are expressed throughout the central nervous system and peripheral tissues of multicelled organisms in which they influence sleep, arousal, feeding and metabolism.
In the last decade, researchers start to analyse their function in health and disease at the cellular and molecular level.
Origins of the circadian clocks
The correspondence between biological and geophysical phenomena was not recognized until the early 1700s, when Jean-Jaques d'Ortous De Marain, a french astronomer, demonstrated that the leaves of Mimosa Pudica continue to open and close every 24 hours even when the plant was enclosed in a sealed box.
Since then, nearly all forms of life on the surface of the planet have been shown to exhibit similar circadian cycles, therefore it became necessary defining the characteristics of biological clocks: a persistent and sustained period lenght under constant conditions, entrainment to environmental signals such as light, and stability across wide variations in temperature.
In human, a first understanding of the phenomena was not based on scientific informations but simply on common facts; the so called Chronotypes emerged from the early 20th century, and divided the population in two groups: some people are “larks” and wake up early, whereas others are “night owls” and stay up late, hinting that there is a biological driver of sleep-wake rhythms.
A triumph of modern genetics has been the identification of the molecular pathways that dictate the sleep-wake cycle and other 24-hour-circadian rhythms.
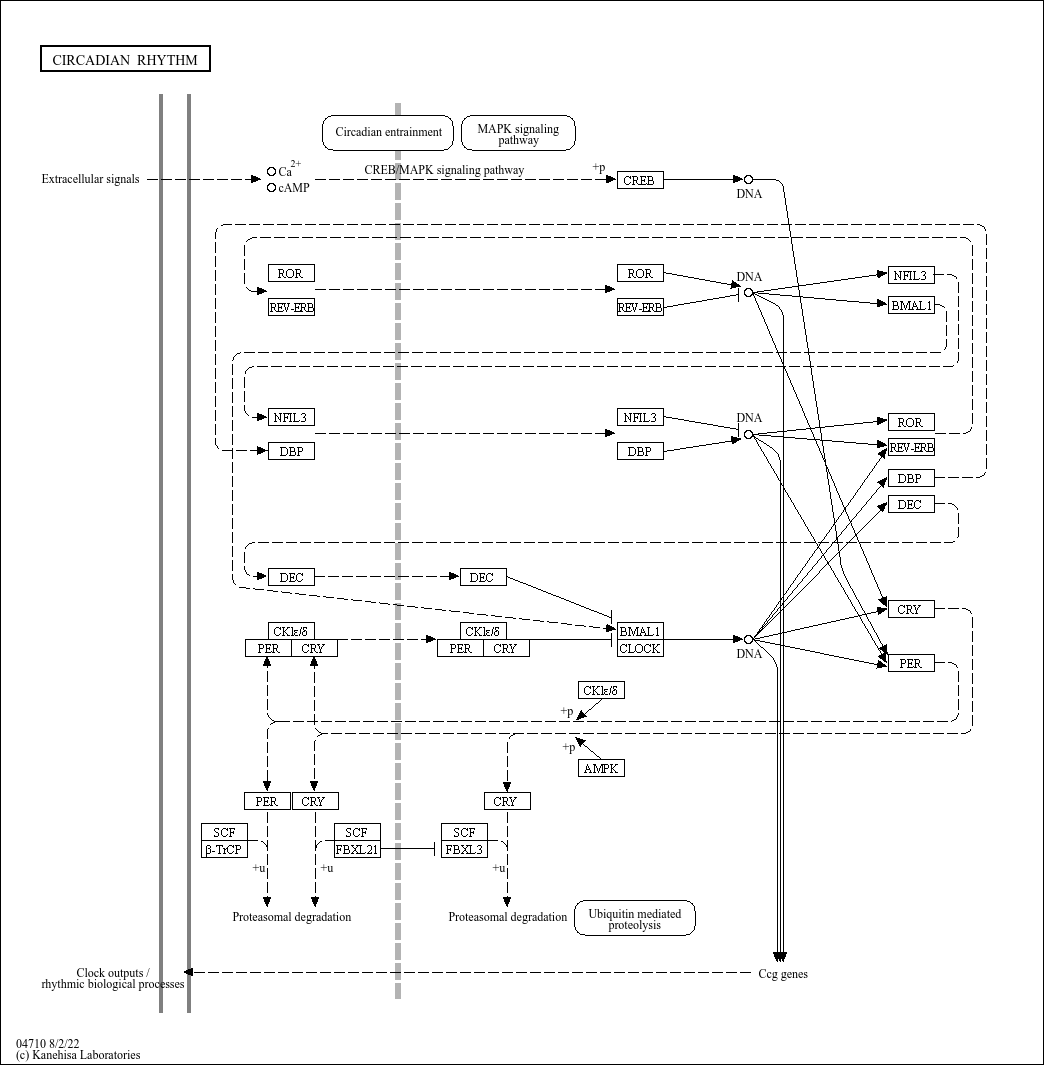
A key advance in circadian genetics was the concept that clocks comprise a transcription autoregolatory feedback loop, with the forward limb encoding activators that promote transcription of a set of repressors, which feed back to inhibit expression and functions.
Indeed, transcriptional oscillators may have provided a selective advantage early in evolution by averting the DNA-damaging effects of sunlight. The presence of a photolyase domain in clock repressors indicates that the timing system co-evolved with DNA repair.
A remarkable series of experiments, such as Light driven changes in energy metabolism directly entrain the cyanobacterial circadian oscillators;2011 , has provided the most convincing evidence for a protein-based clock: a complex of just three protein (KaiA, KaiB, KaiC) together with ATP undergo a self-sustaining 24 hour cycle of alternating phosphorylation and dephosphorylation.
The turnover of ATP modulates the Kai phosphorylation cycle, suggesting that the clock may be coupled to metabolic activity.

An interdependence between circadian and metabolic oscillators has also been suggested by showing that the activity of clock transcription factors is sensitive to redox state; 2011
p=. 
More recently, periodic flux in metabolic cycles has been related to production of reactive oxygen species (ROS).
Peroxiredoxin is a redox-sensitive protein, which has a reactive thiol within the active site that is involved in electron transfer from reactive oxygen.
These proteins exhibit 24-hour oscillation in cells, and this cycle is one of the most conserved among species.
Given that eukaryotes first diverged from bacteria around 1.5 billion years ago, a provocative speculation is that oxygenation of the atmosphere conferred ad adaptive advantage on organism with redox-based clock.
In mammals, oscillation in the Prx redox state have been proposed to represent a means of rhytmically anticipating the generation of ROS.
So, if organism are capable of extinguishing ROS, they may have a survival advantage during the oxygen expansion of the atmosphere.
Consideration of the origins of interal clock remains central to our understanding of links between circadian and metabolic systems.
Clocks impact on fitness in multicellular organisms
A principle to emerge from genetic studies is that period lenght is genetically programmed: but how and why are the body's internal clocks set to 24 hours?
Studies such as Plant circadian clocks increase photosynthesis, growth, survival, and competitive advantage;2005 show that bacteria and plants monitored growth and reproduction under conditions in which alignment between “internal clock” and environmental light cycle and show an advantage to period alignment.
So, it became necessary to understand what are the consequences of misalignment at the molecular level: one possibility is that misalignment reduces genome stability by shuffling the phase relationship between cycles of DNA damage and repair, a second hypothesis is that misalignment may superimpose incopatible biochemical processes, such as the oxidative and reductive phases of the metabolic cycle.
For istance, in Saccharomyces cerevisiae , the mutation rate increases when metabolic cycles are misaligned with DNA replication: it is tempting to speculate that the coupling of DNA repair to circadian cycles may contribute to ageing even in higher eukaryotes.
Neural-clock sensory circuit and circadian-system ageing
Understanding how complex organisms detect light and synchronize the clocks in brain and other tissues to environment remains a central challenge in circadian research.
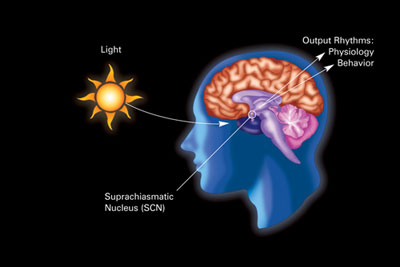
Sensory pathways within the brain have been identified that synchronize the clock independently of visual image formation.
Studies show that even mice without the classic rod and cone visual photoreceptors are still able to synchronize their internal clock to light: the light photoreceptors are expressed in a small number of retinal cells that express the photopigment melanopsin.
Mice that are genetically depleted of these few hundred cells still have normal vision, but they are unable to synchronize their clocks to light: all connections to the hypothalamic pacemakers neurons in the suprachiasmatic nucleus go through these few melanopsin cells.
Suprachiasmatic-nucleus neurons are called the “Master Clock” which synchronizes the hypothalamic control of energy balance, sympathetic outflow and the neuroendocrine systems.
Hypothalamic networks link circadian and energetic centres
The next question is how does the hypothalamic clock communicate with extra-pacemaker and peripheral tissues to produce a coherent phase in the circadian systems throughout the organism?
An appreciation of the central role of the suprachiasmatic nucleus in coordinating sleep-wake behaviour was tested by neural transplantation by using a mutant strain of hamster that shows a short circadian period; 1990 neural grafts from the suprachiasmatic region restored circadian rhythms to arrhythmic animals whose own nucleus had been ablated. The restored rhythms always exhibited the period of the donor genotype regardless of the direction of the transplant or genotype of the host.
These studies also suggested that secreted factors from the suprachiasmatic nucleus contribute to the synchronization of clocks.
Among the areas receiving suprachiasmatic nucleus projections, a large output is toward the lateral hypothalamic area: the nucleus projections synapse on orexin-expressing neurons.
Orexin is neuropeptide that regulates arousal,wakefulness, and appetite: deficiency of either orexin or its receptos is a hallmark of human autoimmune forms of narcolepsy.
Interestingly, narcolepsy is also correlated with elevated body-mass index.
Furthermore, studies such as Low cerebrospinal fluid hypocretin (Orexin) and altered energy homeostasis in human narcolepsy;2001 show that the ablation of orexin receptors increased susceptibilty to died-induced obesity, suggesting that the physiological role of the orexins is to promote arousal and antagonize weight gain.
Ageing and the circadian system
Given the extensive integration of neuroendocrine and circadian systems, it is intriguing to note that suprachiasmatic nucleus function declines with age.
Deficiency of cryptochrome, a repressor of the internal clock repressor, has also been associated with alterations in liver rigeneration, emphasizing the coupling of circadian and cell-cyle pathways.

Cryptochromes are are a class of blue light-sensitive flavoproteins found in plants and animals: the two genes Cry1 and Cry2 code for the two cryptochrome protein CRY1 and CRY2.
In mammals, CRY1 and CRY2 act as light-independent inhibitors of CLOCK - Bmal1 components of the circadian clock.
Circadian origins of metabolic disease
An emerging theme in both circadian and metabolic studies is that it is not only the central nervous system, but also the peripheral tissues that modulate sensory response to the environment.
- Mounting evidence suggests that alignment between central behavioural rhythms and feeding time is important in metabolic health: e.g. Mice fed with a high-fat diet exclusively during the rest period have accelerated weight gain compared with animals fed with the same diet but during the correct circadian time. Circadian timing of food intake contributes to weight gain;2009
An important goal will be to elucidate the neural and molecular basis of the links between altered timing and behavioural and metabolic disruption: indeed alterations in the time of feeding may induce desynchrony between suprachiasmatic nucleus firing rhythms and imput from peripheral feeding responsive signals.
Function of clock genes in metabolic and vascular disease
Genetic tools to perturb the internal clock have created opportunities to analyse the molecular basis of the clustering of certain pathologies such as morning myocardial infarction and hypertensive crises.
Plasminogen activator inhibitor type 1 or PAI-1 is a major physiologic regulator of the fibrinolytic system and has recently gained recognition as a modulator of inflammation and atherosclerosis. PAI-1 exhibits circadian rhythmicity in its expression, peaking in the early morning, which is associated with increased risk for cardiovascular events, The orphan nuclear receptor Rev-erb alpha regulates circadian expression of plasminogen activator inhibitor type 1; 2006
Both autonomous and non-autonomous vascular effects of the clock cause variation in blood pressure across the ligh-dark cycle; CLOCK expression in the vasculature affects the progression of atherosclerosis, Tissue-intrinsic dysfunction of circadian clock confers transplant arteriosclerosis; 2011

The process of circadian synchronization is analogous to protein folding dynamics, with energy minima across the circadian landscape achieved during phase alignment of individual cells and tissues and misalignment (analogous to misfolding traps) induced by either environmental or behavioural perturbation.
Entraining agents promote synchronization and circadian resonance of individual tissue clocks, whereas circadian insults lead to off-synchrony pathways in which phase and amplitude are misaligned. Such misaligned states may be permanent or re-aligned.

Chronobiology and health and management of disease
The integrative physiology of circadian and metabolic systems has emerged through a combination of biochemical and experimental genetic studies.
Monogenic disorders in sleep onset and waking have provided evidence that clocke genes have an effect not only on subjective chronotype, but also on neurological pathways that regulate sleep in humans.
For example, here there are some implications derived from studies about circadian disorders in humans:
- A mutation in human Period 2 or hPER2 a gene crucial for resetting the central clock in response to light, is associated with familial advanced sleep phase syndrome (FASPS), an autosomal dominant condition in which patients feel very sleepy and go to bed early in the evening (e.g. 6:00–8:00 p.m.) and wake up very early in the morning (e.g. around 3:00 a.m.). When someone has advanced sleep phase disorder their melatonin levels and core body temperature will cycle hours earlier than the average person.
For extra information about Circadian Sleep Disorders
But maybe the most important results derived from circadian studies are those concerning with metabolic disorders:
For extra information about Cancer and Circadian Rhythms
The Social Jet Lag
The public health implications ,as we can see, may be quite broad given the frequency of circadian behavioural disruption; indeed, the "Social Jet Lag" that is habit of altering bedtime on weekend has been associated with increased body weight, Social Jet Lag and Obesity, 2012
Obesity has reached crisis proportions in industrialized societies, and many factors converge to yield increased body mass index (BMI): among these is sleep duration. The circadian clock controls sleep timing through the process of entrainment. Chronotype describes individual differences in sleep timing, and it is determined by genetic background, age, sex, and environment (e.g., light exposure).
Social jetlag quantifies the discrepancy that often arises between circadian and social clocks, which results in chronic sleep loss.
The circadian clock also regulates energy homeostasis, and its disruption, as with social jetlag, may contribute to weight-related pathologies.

The models included age, sex, and average sleep duration as variables along with social jetlag and chronotype. Analyses confirmed previous findings, showing that age, sex, and sleep duration are important factors in predicting BMI in both weight groups. For individuals in the normal group, social jetlag is not a predictor for BMI (B). In contrast, living against the clock increases BMI in the overweight group, as exemplified by the positive association between BMI and social jetlag. In this case, the influence of social jetlag is more than half of the impact of sleep duration.
These results demonstrate that living “against the clock” may be a factor contributing to the epidemic of obesity.
This is of key importance in pending discussions on the implementation of Daylight Saving Time and on work or school times, which all contribute to the amount of social jetlag accrued by an individual.
Improving the correspondence between biological and social clocks will contribute to the management of obesity.
In conclusion, at this link you can find a simple and clear video about social jet lag.