Manuele Floreno, Matteo Castronovo
Anesthesia, from Greek ἀναισθησία (an-: "without", and aesthesis: "sensation"), generally means the abolition of sensitivity and pain associated with muscle relaxation.
In medicine it is used to block reversibly sensitivity to pain and skeletal muscle reflexes during surgery or in an invasive procedure.
This procedure has several techniques that differ from each other depending on the type of intervention they are addressed and main ones are:
- General anesthesia, which affects the entire body;
- Local anesthesia, used to operate on small areas such as a tooth or on surface areas of the skin;
The anesthesia exerts its action through the administration of different anesthetic agents.
It is essential in any type of surgery, as it allows patients to undergo operations and other procedures (CAT, endoscopy) without pain, anxiety, and protecting the body from the trauma of the intervention.
General anesthesia or narcosis is a state of pharmacologically induced coma, temporary and reversible, which induces the patient's suppression of consciousness (hypnosis), the abolition of pain (analgesia), the abolition of memory (amnesia) relaxation of the muscles (myorelaxation), and the loss of control of the autonomic nervous system reflexes. Its major applications involve surgery.
The
anesthetic technique consists of some phases: premedication, stages of anesthesia, induction, maintenance and emergence.
- Premedication which consists of a drug or combination of drugs that serve to complement or otherwise improve the quality of the anesthetic. Initially characterized by a visit of the patient by the anesthetist; by means of an interview, the specialist is aware of the patient's medical history, so he can choose the technique of anesthesia more suitable. Finally, about 45 minutes prior to surgery, the patient is given a pre-anesthesia, a set of drugs that decrease anxiety, agitation and allow, therefore, a narcosis easier and safer. This step makes the subject sedated and drowsy, avoid post-operative vomiting, promotes the induction of anesthesia. Among the most widely used drugs in premedication include: anticholinergics (atropine), analgesics (morphine) and neuroleptics (antihistamines).
- Stages of anesthesia:
- Stage 1: induction agents and loss of consciousness. During this stage, the patient progresses from analgesia without amnesia to analgesia with amnesia.
- Stage 2, also known as the "excitement stage", is the period following loss of consciousness and marked by excited and delirious activity. During this stage, respiration and heart rate may become irregular. In addition, there may be uncontrolled movements, vomiting, breath holding, and pupillary dilation. Rapidly acting drugs are used to minimize time in this stage and reach stage 3 as fast as possible.
- Stage 3, "surgical anesthesia". During this stage, the skeletal muscles relax, vomiting stops and respiratory depression does occur . Eye movements slow, then stop, the patient become unconscious and ready for surgery. This stage has been divided into four planes:
- eyes initially rolling, then becoming fixed
- loss of corneal and laryngeal reflexes
- pupils dilate and loss of light reflex
- intercostal paralysis, shallow abdominal respiration
- Stage 4, also known as "overdose", is the stage where too much medication has been given relative to the amount of surgical stimulation and the patient has severe brain stem or medullary depression. This results in a cessation of respiration and potential cardiovascular collapse. This stage is lethal without cardiovascular and respiratory support.
- Induction: anesthetic agents may be administered by various routes, including inhalation, injection (intravenous, intramuscular or subcutaneous), oral, and rectal. After administration, the agents gain access to the blood. Once in the circulatory system, they are transported to their biochemical sites of action in the central and autonomic nervous systems, where they exert their pharmacologic effects. Most general anesthetics today are induced either with a needle, by intravenous injection, or by breathing a volatile anesthetic. Onset of anesthesia is faster with intravenous injection than with inhalation. This has the advantage of avoiding the excitatory phase of anesthesia, and thus reduces complications related to induction of anesthesia. Commonly used intravenous induction agents include propofol, ketamine and curare. An inhalational induction may be chosen by the anesthetist where intravenous access is difficult to obtain, or due to patient preference (e.g., children). Sevoflurane is currently the most commonly used agent for inhalational induction, because it is less irritating to the tracheobronchial tree than other volatile anesthetic agents.
Modern anesthetists have at their disposal a variety of muscle relaxants for use in anesthesia. The ability to produce muscle relaxation independently from sedation has permitted anesthetists to adjust the two effects separately as needed to ensure that their patients are safely unconscious and sufficiently relaxed to permit surgery. Muscle relaxants work by preventing acetylcholine from attaching to its receptor. Acetylcholine, the natural neurotransmitter substance at the neuromuscular junction, causes muscles contraction when it is released from nerve endings. The effects of muscle relaxants are commonly reversed at the termination of surgery by anticholinesterase drugs.
- Maintenance: the duration of action of intravenous induction agents is in general 5 to 10 minutes, after this time spontaneous recovery of consciousness will occur. In order to prolong anesthesia for the required duration (usually the duration of surgery), anesthesia must be maintained. Usually this is achieved by allowing the patient to breathe a carefully controlled mixture of oxygen, nitrous oxide, and a volatile anesthetic agent or by having a carefully controlled infusion of medication, usually propofol, through an intravenous catheter. Inhaled agents are frequently supplemented by intravenous anesthetics.
- Emergence is the process of return to baseline physiologic function of all organ systems after the cessation of administration of general anesthetic agents.
In techniques of intravenous and inhalational inductions are used different anesthetic agents.
Most commonly used intravenous induction agents include propofol, ketamine and curare.
Propofol, marketed under the name of
Diprivan, has largely replaced sodium thiopental (
Pentothal) for induction of anesthesia because recovery from propofol is more rapid and "clear" when compared with Pentothal. Propofol has been proposed to have several mechanisms of action, for example enhances the activity
GABAA receptor, an ionotropic receptor and ion channel sites in the membrane of neurons. Its endogenous ligand is γ-aminobutyric acid (
GABA), one of main neurotransmitters in central nervous system. Upon activation, the
GABAA receptor selectively conducts chloride through the membrane, resulting in hyperpolarization of the neuron. Regulator sites of
GABAA receptor are the target of this agent: the net effect is typically inhibitory, reducing neuronal activity.
Propofol also acts as a sodium channel blocker thus stopping the entry of the ion in the cell and inhibiting nerve stimulation.
Ketamine is
a non-competitive N-methyl D-Aspartate (
NMDA) antagonist. More specifically, ketamine binds the allosteric site of the
NMDA receptor inhibiting its channel. Ketamine's action interferes with pain transmission in the spinal cord preventing central sensibility.
Ketamine also:
- acts on nitric oxide synthase, inhibiting production of nitric oxyde involved in pain perception contributing to analgesia.
- blocks voltage-sensitive calcium channels and depresses sodium channels, attenuating hyperalgesia.
Curare was the first drug used as a neuromuscular blockade that blocks the nicotinic acetylcholine receptor (nAChR), one of the two types of acetylcholine (ACh) receptors, at the neuromuscular junction. Curare occupies the same position of Ach on the receptor with an equal or greater affinity, and elicits the inhibition of this receptor. The antidote for curare poisoning is an acetylcholinesterase (AChE) inhibitor (anti-cholinesterase). Blocking ACh degradation, AChE inhibitors raise the amount of ACh in the neuromuscular junction; the accumulated ACh will then correct the effect of curare because of the bond with the receptors not blocked by toxin.
Main inhalational induction agents include
sevoflurane, an ether often administered in a mixture of nitrous oxide and oxygen. With another volatile anesthetic, desflurane, has the fastest onset and offset. Sevoflurane is the preferred agent for its lesser irritation to mucous membranes. There aren’t well known mechanisms of action for this drug that seem it has been implicated in neuronal degeneration. This activity is thought as an inhibition of
NMDA receptors or an interference of
GABA neurotransmission.
Anesthesia awareness occurs during general anesthesia, on the operating table, when the patient has not been given enough of anesthetic or analgesic to render the patient unconscious during operation (often when agents used to paralyze the patient have been administered). In brief, it is the post-operative recall of intra-operative events.
The incidence of this anesthesia complication is variable and seems to affect 0.2% to 40% of patients according to the surgical setting carried out. In this situation, the patient may feel the pain or pressure of surgery, hear conversation or experience air hunger or difficulty breathing caused by intubation errors and/or problems with the ventilator. If anesthesia awareness occur, about 42% of patients feel the pain of the operation, 94% experience panic and anxiety (sometimes due to impossibility in breathing) because they have not been warned that they will be paralyzed. The patient may be unable to communicate any distress because he has been given a muscle relaxant that acts as a paralyzing in order to facilitate tracheal intubation. A fully paralyzed patient is unable to move, speak, blink the eyes, or otherwise respond to the pain. It is incorrect to think that physiological signs such as increased heart rate (
tachycardia), blood pressure (
hypertension), dilation of the pupils (
mydriasis), sweating (
diaphoresis), and the formation of tears (
lacrimation) will continue to occur normally in response to pain in the anesthetized state: the neuromuscular blocking drugs used cause skeletal muscle paralysis and interfere with the functioning of the autonomic nervous system. The patient cannot signal his distress and it may not exhibit the signs of awareness that would be expected to be detectable by clinical vigilance.
Post-operative interview by an anesthetist is common practice to elucidate if awareness occurred in the case. If awareness is reported a case review is immediately performed to identify machine, medication, or operator error.
During anesthesia there can be different type of awakening:
- subconscious intra-operatory awakening accompanied with amnesia: the patient doesn’t awake completely and he doesn’t remember voices or events who have assisted.
- completely conscious awakening with amnesia: the patient is wakeful and respond to verbal commands such as opening or closing eyes, but in post-operation he doesn’t remember anything. However, under hypnosis, the patient can recollect the intra-operative events.
- conscious awakening without amnesia: in this case the patient experiences all the anguish and fear of a state of apparent death, of a functioning brain in a motionless body, lifeless, which can neither speak nor breathe independently, just like in the classic horror movie.
Most cases of awareness are caused by inexperience and poor anesthetic technique. Very rare causes of awareness include drug tolerance, or a tolerance induced by the interaction of other drugs. There are several possible reasons for this: lower alcohol consumption, female hormones, differential fat distribution in the body, but nobody has researched this. Younger age, obesity, tobacco smoking, or long-term use of certain drugs (alcohol, opiates, or amphetamines) may increase the anesthetic dose needed to produce unconsciousness. There may be genetic variations that cause differences in how quickly patients clear anesthetics, and there may be differences in how the sexes react to anesthetics as well. Marked anxiety prior to the surgery can increase the amount of anesthesia required to prevent recall.
Recent
advances have led to the manufacture of monitors of awareness. Typically these monitor the
electroencephalography (EEG), which represents the electrical activity of the cerebral cortex, which is active when awake but quiescent when anesthetized (or in natural sleep). These newer technologies also include the
bispectral index (BIS) which purport to monitor the depth of anesthesia. Titrating anesthetic agents to a specific bispectral index during general anesthesia allows the anesthetist to adjust the amount of anesthetic agents to the needs of the patient.
Local anesthesia inhibits sensory perception within a specific location on the body, such as a tooth. It is based on local anesthetics.
Clinical local anesthetics belong to one of two classes: aminoamide and aminoester.
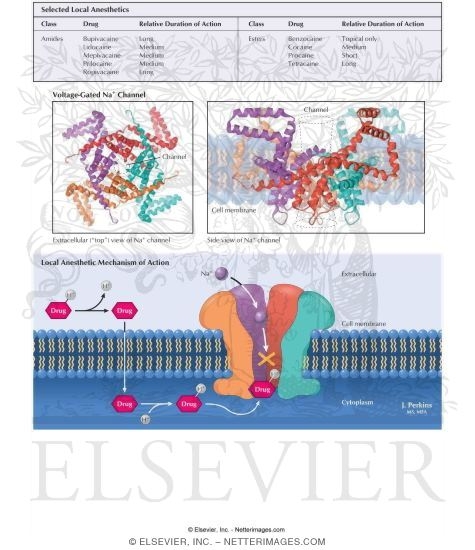
All local anesthetics are membrane stabilizing drugs; they reversibly decrease the rate of depolarization and repolarization of excitable membranes. Local anesthetic drugs act mainly by inhibiting sodium influx through its channels in the neuronal cell membrane, in particular the so-called voltage-gated sodium channels. When the influx is interrupted, the action potential cannot arise and signal conduction is inhibited. The receptor site for these drugs is located at the cytoplasmic portion of the sodium channel. Local anesthetic agents bind more readily to sodium channels in an activated state, thus onset of neuronal blockade is faster in neurons that are rapidly firing.
Local anesthetics are weak bases and are usually formulated with the hydrochloride salt to render them water-soluble: the protonated and unprotonated forms of the molecule exist in equimolar amounts but only the unprotonated base diffuses quickly across cell membranes. Once inside the cell the local anesthetic will be in equilibrium, with the formation of the protonated form, which does not readily pass back out of the cell: this is referred to as "ion-trapping". In protonated form, the molecule binds the local anesthetic binding site on the inside of the ion channel.
Acidosis such as inflammation caused by a wound partly reduces the action of local anesthetics because most of the anesthetic is ionized and therefore unable to cross the cell membrane to reach its cytoplasmic-facing site of action on the sodium channel. All
nerve fibers are sensitive to local anesthetics, but in order to major sensibility there are gamma and delta fibers, followed by alpha and beta fibers, and then by type B and type C fibers.
Techniques
The most peripheral technique is topical anesthesia to the skin or other body surface. Small and large peripheral nerves can be anesthetized individually (peripheral nerve block) or in anatomic nerve bundles (plexus anesthesia). Spinal anesthesia and epidural anesthesia merges into the central nervous system.
Injection of local anesthetics is often painful. A number of methods can be used to decrease this pain including buffering of the solution with bicarbonate and warming.
Clinical techniques include:
- Surface anesthesia - application of local anesthetic spray, solution or cream to the skin or a mucous membrane. The effect is short lasting and is limited to the area of contact.
- Infiltration anesthesia - injection of local anesthetic into the tissue to be anesthetized. Surface and infiltration anesthesia are collectively topical anesthesia.
- Peripheral nerve block - injection of local anesthetic in the vicinity of a peripheral nerve to anesthetize that nerve's area of innervation.
- Plexus anesthesia - injection of local anesthetic in the vicinity of a nerve plexus, often inside a tissue compartment that limits the diffusion of the drug away from the intended site of action. The anesthetic effect extends to the innervation areas of several or all nerves stemming from the plexus.
- Epidural anesthesia - a local anesthetic is injected into the epidural space where it acts primarily on the spinal nerve roots. Depending on the site of injection and the volume injected, the anesthetized area varies from limited areas of the abdomen or chest to large regions of the body.
- Spinal anesthesia - a local anesthetic is injected into the cerebrospinal fluid, usually at the lumbar spine (in the lower back), where it acts on spinal nerve roots and part of the spinal cord. The resulting anesthesia usually extends from the legs to the abdomen or chest.
Local anesthesia is used in dentistry in case of need of surface anesthesia, infiltration anesthesia or intra-ligamentary anesthesia during restorative operations or extractions, regional nerve blocks during extractions and surgeries.
The local adverse effects of anesthetic agents include neurovascular manifestations such as prolonged anesthesia (numbness) and paresthesia (feeling of "pins and needles", or strange sensations). These are symptoms of localized nerve impairment or nerve damage. These agents may generate adverse effects also in the central nervous system and the heart, Additionally, patients may exhibit allergenic reactions to the anesthetic compounds and may also exhibit cyanosis due to methemoglobinemia.
Esters are prone to producing allergic reactions, which may necessitate the use of an Amide. The names of each locally clinical anesthetic have the suffix "-caine". Most ester local anesthetics are metabolized by pseudocholinesterases, while amide local anesthetics are metabolized in the liver. This can be a factor in choosing an agent in patients with liver failure.
Complication of Local Anesthetics Used: Paresthesia
Paresthesia or persistent anesthesia is a complication that leads the patient to feel the area anesthetized numb for several hours or days after the injection of local anesthetic. It is a complication often not predictable and is one of the most frequent lawsuit medico-legal. In dental clinical, symptoms present with numbness, swelling, tingling, itching, which may be associated with disorders such as biting the tongue, loss of taste and saliva, speech disorder.
Most principal causes for this condition in dentistry include:
- The injection of a local anesthetic contaminated by alcohol (it is a neurolitic substance) or by sterilizing solution closeness of the nerve which causes irritation accompanied by edema and increase of pressure in the region with consequent paresthesia.
- The insertion of the needle into a foramen of the maxillary block.
- Hemorrhage around or within the nerve sheath: the bleeding fact leads to an increase in pressure on the nerve resulting in paresthesia.
- Also the concentration of local anesthetic administered can influence the paresthesia. Prilocaine is an example of it: when it is used in 4% there is a higher incidence of paresthesia.
Local Anesthetics
- Vasoconstrictors are fundamental in dentistry because the anesthetic alone, generally, does not provide a sufficient anesthetic duration. The use of vasoconstrictors is more useful in anesthesia by infiltration rather than in the block nervous. The concentrations used are 1:50.000 (indicated especially in surgery when you want to have even a good hemostatic effect) and 1:100,000 1:200,000.
With their function of vasoconstriction, they slow down the blood flow allowing the anesthetic to act more effectively in a particular region of the body
The vasoconstrictors can interact with many drugs. The use must be limited in presence of significant cardiovascular disease or if patient is taking medications that interact with vasoconstrictors to avoid the risk of ischemia.
Maximum recommended dose of local anesthetic with vasoconstrictor
| Anesthetics |
maximum dose |
maximum number of vials |
| Articaine |
7 mg/Kg (5 mg/Kg in children) |
7 |
| Bupivacaine |
2 mg/Kg |
10 |
| Lidocaine |
7 mg/Kg |
13 |
| Mepivacaine |
6.6 mg/Kg |
11 (7 without vasoconstrictors) |
| Prilocaine |
8 mg/Kg |
8 |
Prilocaine, lidocaine and articaine are some of the local anesthetics used in dentistry:
Prilocaine (amide). It is a local anesthetic of the amino amide type. In its injectable form (trade name
Citanest), it is often used in dentistry. It is also often combined with lidocaine as a preparation for dermal anesthesia for treatment of conditions like paresthesia: solution of lidocaine-prilocaine, also named
EMLA, contains 2.5% each of these agents.
Lidocaine (amide). It is also used in dentistry. It alters signal conduction in neurons by blocking the fast voltage-gated sodium channels in the cell membrane that are responsible for signal propagation. With sufficient blockage the membrane of the postsynaptic neuron will not depolarize and will thus fail to transmit an action potential. This creates the anesthetic effect by not merely preventing pain signals from propagating to the brain but by stopping them before they begin. Careful titration allows for a high degree of selectivity in the blockage of sensory neurons, whereas higher concentrations will also affect other modalities of neuron signaling.
Articaine. It is the most widely used local anesthetic in a number of European countries.
The amide
structure of articaine is similar to other local anesthetics, but its molecular structure differs for the presence of a
thiophene ring instead of a
benzene ring. Articaine is exceptional because it contains an additional ester group that is metabolized by estearases in blood and tissue. Since articaine is hydrolyzed very quickly in the blood, the risk of systemic intoxication seems to be lower than with other anesthetics, especially if repeated injection is performed.
This agent
is used for pain control and causes a transient and completely reversible state of anesthesia (loss of sensation) during (dental) procedures.
In an article by Haas and Lennon published in 1993 they seem to settle the controversy surrounding articaine.
This paper, analyzed 143 cases reported in to the Royal College of Dental Surgeons of Ontario (RCDSO) over a 21-year period. The results from their analysis seemed to indicate that 4% local anesthetics had a higher incidence of causing paresthesia, an undesirable temporary or permanent complication, after the injection. If paresthesia does occur, the results of this study are consistent with the suggestion that it is significantly more likely to do so if either articaine or prilocaine is used.
In another paper by the same authors, 19 reported paresthesia cases in Ontario in 1994 were reviewed, concluding that the incidence of paresthesia was 2.05 per million injections of 4% anesthetic drugs. Another follow up study by Miller and Haas published in 2000 concluded that the incidence of paresthesia from either prilocaine or articaine (the only two 4% drugs in the dental market) was close to 1:500,000 injections (an average dentists gives around 1,800 injections in a year).
Almost all recorded cases of long term of numbness or altered sensation (paresthesia) seem to only be present when this anesthetic is used for dental use (no PubMed references for paresthesia with articaine for other medical specialties), and only affect, in the vast majority of the reports, the lingual nerve. Nonetheless, direct damage to the nerve caused by 4% drugs has never been scientifically proven, in fact some research points to needle trauma as the cause of the paresthesia events.