IODINE METABOLISM

Effect of oxygen concentrations on sodium iodide symporter expression and iodide uptake and hCG expression in human choriocarcinoma BeWo cells. - PubMed - NCBI
h3. IODINE
Iodine is a micronutrient of crucial importance for the health and well-being of all individuals. Iodine is mostly concentrated in thyroid gland.
A healthy adult body contains 15-20 mg of iodine, 70-80% of which is stored in the thyroid gland.
Daily intake of iodine by an individual amounts to 500 micrograms; daily physiological requirement during adult life is 150 micrograms; during pregnancy and lactation period is 200 micrograms; and during neonatal period is 40 micrograms. Normally about 120 micrograms of iodide are taken up by the thyroid gland for the synthesis of thyroid hormones t3 and t4.
Diet is the sole source of iodine, that is mostly obtained from food sources particularly vegetables grown on iodine-rich soil; the remaining requirement is met from drinking water.
The World Health Organization has identified iodide deficiency as a leading cause of brain damage worldwide. More than 1.2 billion people are estimated to lack sufficient access to iodide despite our very modest daily requirement for this micronutrient. Iodide uptake is a critical first step in thyroid hormone synthesis.
Ingested iodine is bound to serum proteins, particularly albumin .
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3104944/?report=classic
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2568863/
Unbound iodine is excreted in the urine. The thyroid gland extracts iodine from the circulation in a highly efficient manner. For example, 10–25% of radioactive tracer (e.g., 123I) is taken up by the normal thyroid gland over 24 hours; this value can rise to 70–90% in Graves' disease. With Graves' disease, the immune system makes antibodies that act like TSH, causing the thyroid to make more thyroid hormone than your body needs. The thyroid gland plays a central role in the metabolism of iodine.
IODINE TRAPPING
Iodine trapping is the first step in the metabolism of iodine.
The process commences with the uptake of iodide from the capillary into the follicular cell of the gland by an active transport system. This occurs against chemical and electrical gradients by sodium / iodine symported protein (NIS) found in the basolateral membrane of the follicular cell; the energy required by this process is linked to the ATPase dependent Na- K pump. NIS is most highly expressed in the thyroid gland, but low levels are present in the salivary glands, lactating breast, and placenta.
The iodide transport mechanism is highly regulated, allowing adaptation to variations in dietary supply.
Low iodine levels increase the amount of NIS and stimulate uptake, whereas high iodine levels suppress NIS expression and uptake. The selective expression of NIS in the thyroid allows isotopic scanning, treatment of hyperthyroidism , and ablation of thyroid cancer with radioisotopes of iodine, without significant effects on other organs. Mutation of the NIS gene is a rare cause of congenital hypothyroidism ,underscoring its importance in thyroid hormone synthesis.

THYROGLOBULIN SYNTHESIS
Synthesis and secretion of thyroglobulin is the second step. It occurs by another independent process within the follicular cell; the synthesis starts on the rough endoplasmic reticulum as peptide units of molecular weight 330,000 (the primary translation product of its messenger RNA). Later these units combine into a dimer, followed by addition of carbohydrate moieties, after which the molecule moves to the Golgi apparatus. The completed thyroglobulin molecule, that is a large (660 kDa) dimeric protein that consists of 2769 amino acids, contains about 140 tyrosine residues, which serve as substrate for the synthesis of thyroid hormones, is contained within small vesicles which then move towards the apical surface of the plasma membrane before being released into the follicular lumen.
IODIDE’S OXIDATION
The third step is the oxidation of iodide. The iodide within the follicular cell moves towards the apical surface of the plasma membrane, to enter into the follicular lumen; this transport by a iodide/chloride transporter called pendrin. The iodide (I') is then immediately oxidized to Iodine (I). This is followed by organification of the thyroglobulin, wherein iodination of the tyrosine residues present within the thyroglobulin molecule occurs.
Iodination first occurs at position 3 to form monoiodotyrosine (MIT) and then at position 5 to form diiodityrosine (DIT). Iodination of tyrosine is followed by coupling reaction, whereby, two molecules of DIT couple to form thyroxine (T4) hormone; and one molecule of MIT couples with one molecule of DIT to form Triiodothyronine (T3) hormone.
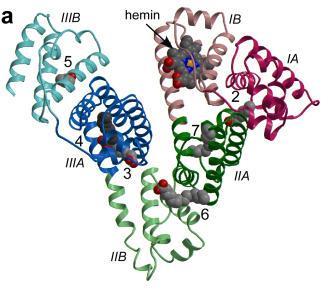
The reaction is catalyzed by thyroid peroxidase (TPO ) that is a membrane-bound, glycosylated, heme-containing protein located on the apical membranes of the thyroid follicular cell. The organification of iodine requires the presence of molecular oxygen which is supplied by hydrogen peroxide that is generated by the enzyme of the apical membrane DUOX, family of NADPH oxidase that catalyses the transfer of one electron from NADPH to molecular oxygen, resulting in the formation of superoxide.
The oxidation of iodide occurs at the interface between the apical membrane and colloid.
The reactive iodine atom is added to selected tyrosyl residues within Thyroglobulin.
TPO. catalyses the reaction:
2 L-Tyrosin + 2 I− + H2O2 ⇒ 2 3-Iod-L-Tyrosin + 2 H2O
Iodide is oxidized to iodine radical which immediately reacts with tyrosine.
2 3-Iod-L-Tyrosin + 2 I− + H2O2 ⇒ 2 3,5-Diiod-L-Tyrosin + 2 H2O
The second iodine atom is added in similar manner to the reaction intermediate 3-iodotyrosine.
TPO is stimulated by TSH, which upregulates gene expression.
TPO is inhibited by the thioamide drugs, such as propylthiouracil and methimazole.
TPO is predicted to have four modular domains, molecular abnormalities causing defective TPO activity lead to profound congenital hypothyroidism and goitre and because of the biosynthetic defect, the gland is incapable of synthesizing adequate amounts of hormone.
Autoimmune thyroid disease is detected most easily by measuring circulating antibodies against TPO and Thyroglobulin. As antibodies to Thyroglobulin alone are uncommon, it is reasonable to measure only TPO antibodies. About 5–15% of euthyroid women and up to 2% of euthyroid men have thyroid antibodies; such individuals are at increased risk of developing thyroid dysfunction. Almost all patients with autoimmune hypothyroidism, and up to 80% of those with Graves' disease ,have TPO antibodies, usually at high levels.
TSI are antibodies that can be measured in bioassays or indirectly in assays for TSH-binding inhibiting immunoglobulins (TBII) that detect antibody binding to the receptor. The main use of these assays is to predict neonatal thyrotoxicosis caused by high maternal levels of TSI in the last trimester of pregnancy.
Serum Tg levels are increased in all types of thyrotoxicosis except thyrotoxicosis factitia caused by self-administration of thyroid hormone. Tg levels are particularly increased in thyroiditis, reflecting thyroid tissue destruction and release of Tg.
The main role for Tg measurement, however, is in the follow-up of thyroid cancer patients. After total thyroidectomy and radioablation, Tg levels should be undetectable; in the absence of anti-Tg antibodies, measurable levels indicate incomplete ablation or recurrent cancer.
HORMONES RELEASE
At the end, the colloid containing iodinated thyroglobulin undergoes endocytosis, whereby it is salvaged from the follicular lumen by the epithelial cells. The colloid now enters the cytoplasm in the form of colloid droplets, which move towards the basal membrane possibly by way of microtubule and microfilament function. The colloid droplets next fuse with lysosome vesicles which contain proteolytic enzymes. The proteases help digest the thyroglobulin molecule releasing T4, T3, DIT and MIT into the cytoplasm. While T4 and T3 diffuse via the basal surface into the blood stream, the MIT and DIT get rapidly deiodinated by enzyme deiodinase. This mechanism helps retrieve iodide for recycling along with tyrosine for recycling.