Definition
Also known as "alarm clock" headache, hypnic headache is characterized by episodes of dull head pain that develop only during sleep and awaken the sufferer from sleep. It is one of the few headache disorders to occur almost exclusively in later life.
Epidemiology
Originally believed to be a disorder of the elderly, subsequent reports suggest that the disorder may begin earlier, but many patients suffer for decades before the diagnosis is made. Later studies reveal that the 65,8% of women suffers from this disease, the ratio women:men is 1,9:1! The 69,9% of clinical cases reveal bilateral pain, the remaining 30,1% unilateral pain. Usually only one crisis affects patients during a sleep, but exceptional cases of multiple crisis exist. Hypnic headache is identified especially in Europe, in North America and in big cities of the other parts of the world, probably related to modern life style.

Symptoms
The pain can be unilateral or bilateral, it is usually mild to moderate, but sometimes severe, it develops during sleep and awakens the sufferer. It usually has a dull quality, although the original paper in 1988 (by Professor Raskin from University of California, San Francisco) described throbbing pains. The pain begins abruptly and can last from 15 minutes to 6 hours, although typically it lasts about 30-60 minutes. The pain is not associated with autonomic features (such as a blocked nose or watering eyes). Similarly, nausea, photophobia and phonophobia are not usually associated with hypnic headache, vomiting is rare. Pain commonly occur at the same time every night possibly linking the headaches with circadian rhythm, but polysomnography has recently revealed that the onset of hypnic headaches may be associated with REM sleep.

Hypnic Headache - The Alarm Clock Headache, 2008-2013
Diagnosis
Diagnostic standards, established by IHS, to identify hypnic headache are:
- Dull headache
- Develops only during sleep, and awakens patient
- At least two of the following characteristics:
- occurs >15 times per month
- lasts ≥15 minutes after waking
- first occurs after age of 50 years
- No autonomic symptoms and no more than one of nausea, photophobia or phonophobia
- Not attributed to another disorder: intracranial disorders must be excluded. Distinction from one of the trigeminal autonomic cephalalgias is necessary for effective management.
IHS Classification ICHD II - Migraine
Pathogenesis
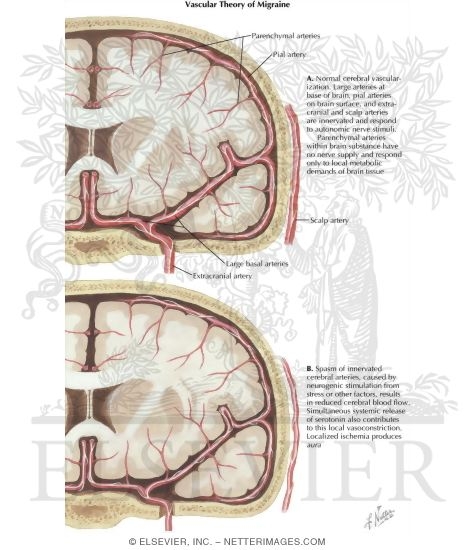
The brain itself is not sensitive to pain, because it lacks pain receptors. However, several areas of the head and neck do have nociceptors, and can thus sense pain. These include the extracranial arteries, large veins, cranial and spinal nerves, head and neck muscles and the meninges. The precise pathogenesis is unknown but some theories has been postulated.
The vascular theory: proposed by Wolff, it described the intracranial vasoconstriction as being responsible for the beginning of the problem. The vasoconstriction is caused by an increase of serotonin in the cerebral vascolar tissue, the headache was believed to result from the subsequent rebound of the dilatation of the blood vessels which led to the activation of the perivascular nociceptive nerves. The developers of this theory took into consideration the changes that occur within the blood vessels outside the cranium when a migraine attack occurs and other data that was available at that time including the effect of vasodilators and vasoconstrictors on headaches.
The vascular theory has problems:
- blood vessels routinely constrict and dilate without causing pain;
- vascular constriction that happens during migraine episodes doesn't choke off cerebral blood flow enough to cause aura symptoms;
- an experiment in which blood pressure in the brain was artificially increased failed to produce migraine-like symptoms;
- the central problem with the vascular theory, however, is that it assumes vascular changes cause migraine symptoms, when there are other logical possibilities: the headache could cause the vascular dilation, or a third factor could cause both the vascular dilation and the headache.
Ipotalamic theory: Commonly patients experience the headache at a predictable time each night, suggesting a link with the circadian rhythm, which is orchestrated by the suprachiasmatic nucleus in the hypothalamus (also involved in antinociception). These nuclei produce, among others, melatonin, an important mediator of circadian rhythm. With advancing age the function of the hypothalamus, and thus melatonin secretion, is impaired. This could also be involved in the pathogenesis of hypnic headache. Lithium is believed to increase melatonin levels and may explain its mode of action.
Sleep-related headache and its management - Pubmed 2013
Patient risk factor
It is known that genetic inheritance plays a part. The general idea is that variable environmental or internal factors act on a genetically inherited predisposition to produce a migraine episode. Three genes associated with familiar hemiplegic migraine, a rare type of primary headache, and a gene linked to the risk for cluster headache are known. Until recently, however, no gene associated with the most common forms of migraine had been identified. The first such association, announced in February 2007, is between migraine with aura and a particular variation in the gene for the type A2a adenosine receptor, probably involved in hypnic headache too.

Certainly age and gender are the most important risk factors. This headache affects especially women with the average age of onset being 63 ± 11 years.
Genome-wide-associated variants in migraine susceptibility: a replication study from north India, Pubmed 2013
Therapy
In addition to classical drugs, like Lithium, Verapamil, Indomethacin or Methysergide, hypnic headache is the only primary headache that is successfully cured by caffeine.
Caffeine is a neurotoxic alkaloid naturally occurring in over 100 species of plants. Presumably, plants manufacture caffeine to discourage insect browsing. Caffeine protects plants by suppressing insect appetite or otherwise inhibiting their ability to eat. For insects, eating is a complicated process that requires precise coordination from a properly functioning nervous system. By interfering with or altering the normal neurochemical functioning of insect nervous systems, caffeine disrupts the intricate nervous mechanisms that enable and control eating.
Which Plants Contain Caffeine?, march 13, 2013
Caffeine Kills Insects, Scientist Says, October 9, 1984
In human brain caffeine works by occupying and blockading adenosine receptors embedded in the surface membranes of neurons (nerve cells). The caffeine molecule (on the left on the pic) is similar in shape to adenosine (on the right). Caffeine molecules fit into adenosine receptors without activating them, so prevent adenosine from binding to adenosine receptors, thereby blocking the action of adenosine.
The effect of coffee on blood pressure at healthy subjects, Pubmed 2013

Adenosine does a lot of things. It's called a neuromodulator, because it modulates, or controls, the activity of neurotransmitting molecules including serotonin, norepinephrine, dopamine, and acetylcholine. The effect adenosine has depends on where in the body the adenosine is; adenosine can have opposite effects in different parts of the nervous system. Overall, adenosine acts as a tranquilizer, inhibiting nerve firing by inhibiting the release of excitatory neurochemicals. Centrally, in the brainstem and spinal cord, adenosine is a painkiller, but peripherally, in the outer reaches of the nervous system, it causes pain. Adenosine applied to the skin causes localized pain and vasodilation. Adenosine dilates blood vessels in the head and neck.
Caffeine, because it blocks adenosine, has the opposite effects of adenosine. Caffeine constricts blood vessels in the head and neck, and increases the release of excitatory neurochemicals, so increases the rate of nerve firing. That's why caffeine is stimulating.
Caffeine has only one known mechanism of action at likely doses: occupation and blockade of adenosine receptors. Whatever the cause of a given primary or secondary headache, if caffeine relieves that headache, it does so by blocking adenosine. That tells us something important about headaches relieved by caffeine: their causal mechanism involves adenosine binding to adenosine receptors.
The concentration of adenosine in the head and neck is increased above normal levels during headache episodes, so adenosine, which causes pain peripherally and is a vasodilator, readily explains the head pain and vascular dilation associated with headache.
That caffeine oftentimes relieves migraine means adenosine must be a key part of the mechanism of headache. This straightforward reasoning makes little impression on headache researchers, though they haven't completely ignored adenosine. In 1996 Professor Burnstock proposed that adenosine is the endogenous (originating within the body) cause of headache pain. Always looking for new drug targets, headache researchers have investigated the possibility of using adenosine receptor agonists, molecules that bind to and activate adenosine receptors, as headache medicines.
There have been several theories that attempt to explain why caffeine relieves headaches. One is that caffeine works by constricting blood vessels. Blood vessels in the head and neck are dilated during a headache episode, and caffeine does indeed constrict blood vessels in the head and neck. The conclusion that caffeine relieves headache by constricting blood vessels, however, is based on the assumption that vascular dilation causes migraine headache. This assumption has its backwards: vascular dilation is a symptom of headache, not the cause of migraine headache. Caffeine's headache-relieving power doesn't depend on its vasoconstrictive effect.
Oftentimes a migraine headache is a pounding headache, with pain spiking in time with the pulse. In some cases, dilated superficial temporal arteries pulsate visibly. These symptoms led migraine theorists in the 1940s to believe vascular dilation and pulsation caused the associated headache pain. The vascular theory of migraine supposes vascular spasms cause migraine symptoms. According to the vascular theory, vascular constriction in the brain causes ischemia (inadequate blood flow causing tissue to be deprived of oxygen), which causes aura symptoms, followed by vascular dilation that causes the head pain. The brain itself is insensitive to pain, so the vascular theory postulates that migraine pain originates when dilated blood vessels in the meninges, the three layers of membrane surrounding the brain, press against or otherwise physically or chemically irritate sensory nerves.
The vascular theory has problems. One is that blood vessels routinely constrict and dilate without causing pain. Another is that the vascular constriction that happens during migraine episodes doesn't choke off cerebral blood flow enough to cause aura symptoms. Yet another is that experiments in which blood pressure in the brain was artificially increased failed to produce migraine-like symptoms. The central problem with the vascular theory, however, is that it assumes vascular changes cause headache symptoms, when there are other logical possibilities: the headache could cause the vascular dilation, or a third, underlying factor could cause both the vascular dilation and the headache.
The vascular theory fails to take into account the neurochemical mechanisms that control vascular constriction and dilation. To understand the relationship between vascular dilation and headache, it's necessary to understand why blood vessels constrict and dilate. Blood vessels are surrounded by a layer of muscle cells that can contract to decrease the diameter of the vessel. The degree to which the muscle layer is contracted is referred to as vascular tone. The layer of muscle cells is under neurochemical control, so the diameter of blood vessels, or vascular tone, is under neurochemical control. The sympathetic nervous system controls blood vessel diameter, and norepinephrine is the final neurotransmitter of the sympathetic nervous system. Norepinephrine constricts blood vessels. Adenosine, by inhibiting the release of norepinephrine from neurons, causes vasodilation. Caffeine, by blocking adenosine, prevents adenosine from inhibiting norepinephrine release, so caffeine increases the amount of norepinephrine released by neurons, and thereby causes vasoconstriction.
The new scientific consensus is that migraine is a neurovascular disorder, the modified idea being that a central nervous system dysfunction leads to the vascular dilation. Many lay authors, however, still assume that the vascular dilation directly generates migraine pain.
Adenosine is the likely culprit behind both the vasodilation and pain. Migraine is a derangement of normal neurochemical mechanisms, including those that control blood vessel diameter. During a migraine episode, the blood concentration of adenosine in the head and neck is elevated quite a bit above normal; by an average of 68 % in one study. Adenosine causes pain and is a potent vasodilator, so it's not surprising that excessive adenosine in the head is associated with the head pain and vascular dilation that typically accompany migraine episodes. Nor is it surprising that caffeine, which blocks adenosine, remedies headache.
So taking a cup of coffee before going to bed can help the hypnic headache patients to improve their life quality.
Caffeine's Vascular Mechanisms of Action., Pubmed 2010
Headaches - 1998-2013 Mayo Foundation for Medical Education and Research
Bibliography
http://en.wikipedia.org/wiki/Main_Page
http://www.nhs.uk/conditions/Watering-eye/Pages/Introduction.aspx
http://ihs-classification.org/en/02_klassifikation/02_teil1/04.05.00_other.html
http://www.ncbi.nlm.nih.gov/pubmed/24132786
http://www.ncbi.nlm.nih.gov/pubmed/24266335
http://www.medscape.com/viewarticle/780334
http://www.thecrimson.com/article/1984/10/9/caffeine-kills-insects-scientist-says-pif/
http://www.ncbi.nlm.nih.gov/pubmed/24224448
http://www.ncbi.nlm.nih.gov/pubmed/21188209
http://www.mayo.edu/research/departments-divisions/department-neurology/programs/headaches
Presciani Damiano