Respiration is defined as the transport of oxygen from the outside air to the cells within tissues, and the transport of carbon dioxide in the opposite direction.
The Oxygen availability to the tissues is expressed as local pO 2
Environmental pO 2

Respiratory System:
- The primary function of the respiratory system is to supply the blood with oxygen in order for the blood to deliver oxygen to all parts of the body and eliminate carbon dioxide that cells produce
- Includes respiratory airways leading into and out of lungs plus the lungs themselves
- Pathway of air: nasal cavities (or oral cavity) > pharynx > trachea > primary bronchi (right and left) > secondary bronchi > tertiary bronchi > bronchioles > alveoli (site of gas exchange)
Breathing includes four stages:
- Ventilation, moving of the ambient air into and out of the alveoli of the lungs.
- Pulmonary gas exchange, exchange of gases between the alveoli and the pulmonary capillaries.
- Gas transport, movement of gases within the pulmonary capillaries through the circulation to the peripheral capillaries in the organs, and then a movement of gases back to the lungs along the same circulatory route.
- Peripheral gas exchange, exchange of gases between the tissue capillaries and the tissues or organs, impacting the cells composing these and mitochondria within the cells
Note that ventilation and gas transport require energy to power a mechanical pump (the heart) and the muscles of respiration, mainly the diaphragm. In heavy breathing, energy is also required to power additional respiratory muscles such as the intercostal muscles. The energy requirement for ventilation and gas transport is in contrast to the passive diffusion taking place in the gas exchange steps.
A. VENTILATION : moving of the ambient air into and out of the alveoli of the lungs
The ambiental air, that we breathe, is a mixture of gases and microscopic particles of solid and liquid. The chemical composition of the atmosphere remains virtually constant even beyond the limits of the troposphere, at least up to 20 km altitude.
The two main components are nitrogen, which forms an almost four-fifths (78.08%) and oxygen which represents just over a fifth (20.94%). The first is a basic element of protein, namely, the fundamental constituents of every living thing and part atmospheric nitrogen is made available to plants through the action of certain soil bacteria, the nitrogen-fixing and the second component is essential for respiration of plants and animals and for combustion.
Then there are the rare gases: argon, neon, helium, krypton, xenon, by reason of 0.94%, and carbon dioxide, which represents only 0.03%. It though present in very small percentages, plays a role vitally important, in fact, green plants absorb carbon dioxide and combine it in the photosynthetic process, with hydrogen to produce water nutrients necessary for their existence and, consequently, also in the lives of all animals, releasing , while oxygen. In addition, the carbon dioxide is an important regulator of the temperature of the Earth because it is transparent to sunlight but absorbs the thermal radiation emitted by the Earth's surface, making it more difficult to scatter energy in space. Carbon dioxide has a strong seasonal variability, the fall foliage in winter raises the amount of carbon dioxide, while in spring the increase in photosynthesis removes carbon dioxide to the atmosphere.
With regard to human life, is extremely important to stress that only the oxygen (1 / 5 of the gases in the atmosphere) is used by our body in more detail can be explained that with the exhalation in reality it still emits a very high quantities of oxygen (air exhausted with 16% oxygen, while that has inspired a concentration of 21%), with use of the then only 5%, and that the percentages of nitrogen and other gases remain unchanged.
In the composition of the air should be considered also other elements:
Water vapour : is present in varied proportions, it derives from evaporation of surface water by the action of heat is normally found in larger quantities above the hot humid climate areas than on the desert or polar regions. When the relative humidity exceeds certain values, there is condensation of water around the particles, condensation nuclei, with the formation of cloud droplets. The air so-called "wet air" may contain up to 7% water vapor, this percentage depends on the relative air humidity and temperature and is limited by the saturation vapor pressure of the water. The highest percentage content depends on temperature, varies from values close to 0% at -40 C, about 0.5% at 0 C, 5-7% at around 40 C.
Gases due to the activities that take place in the atmosphere : most pollutants issued remains confined in the troposphere, some concentrated near the earth's surface, some ozone (O 3), carbon dioxide (CO2), methane (CH 4), are distributed more evenly
The rate of carbon dioxide is highly variable in recent times. In particular, human activity (industry, pollution, combustion, deforestation, etc. ...) have produced a large increase in this percentage over the past century. Hydrogen is also always but in very small quantity, comes from both fermentations that take place on Earth, either from volcanic phenomena.
Intra-alveolar pressure during inspiration & expiration
During inspiration, as the external intercostals and diaphragm contract, the lungs expand. The expansion of the lungs causes the pressure in the lungs (and alveoli) to become slightly negative relative to atmospheric pressure. As a result, air moves from an area of higher pressure (the air) to an area of lower pressure (our lungs and alveoli).
During expiration, the respiration muscles relax and lung volume descreases. This causes pressure in the lungs (and alveoli) to become slight positive relative to atmospheric pressure. As a result, air leaves the lungs.

The walls of alveoli are coated with a thin film of water and this creates a potential problem. Water molecules, including those on the alveolar walls, are more attracted to each other than to air, and this attraction creates a force called surface tension. This surface tension increases as water molecules come closer together, which is what happens when we exhale and our alveoli become smaller (like air leaving a balloon). Potentially, surface tension could cause alveoli to collapse and, in addition, would make it more difficult to 're-expand' the alveoli (when you inhaled). Fortunately, our alveoli do not collapse and inhalation is relatively easy because the lungs produce a substance called surfactant that reduces surface tension.
B. PULMONARY GAS EXCHENGE : exchange of gases between the alveoli and the pulmonary capillaries.
The exchange of gases (O2 and CO2) between the alveoli and the blood occurs by simple diffusion: O2 diffusing from the alveoli into the blood and CO2 from the blood into the alveoli. Diffusion requires a concentration gradient. So, the concentration (or pressure) of O2 in the alveoli must be kept at a higher level than in the blood and the concentration (or pressure) of CO2 in the alveoli must be kept at a lower lever than in the blood.

Pulmonary circulation is the portion of the cardiovascular system which carries oxygen-depleted blood away from the heart, to the lungs, and returns oxygenated blood back to the heart. Pulmonary blood flow is the entire scope of the right ventricle. This blood participates in gas exchange with alveolar air in the pulmonary capillaries and as the right and left ventricles are arranged in series in normal adults, the pulmonary blood flow is approximately equal to 100% range of the left ventricle. That is to say that the pulmonary blood flow equals cardiac output (usually equal to about 3.5 L/min/m2 of body surface area at rest). The amount of blood present in the pulmonary circulation at any moment is about 250-300 ml per m2 of body surface area. 60-70 ml/m2 of this blood are localized in the pulmonary capillaries. During exercise, cardiac output may increase by many times without encountering a corresponding increase in mean pulmonary artery pressure: the recruitment and distension of capillaries are the two phenomena underlying physiological adaptation of the pulmonary circulation.
Pulmonary blood flow is directed away from poorly ventilated regions to better ventilated regions of the lung.
Pulmonary blood pressure, in arteries and capillaries, is low if compared with systemic circulation.
For example at rest:
Systemic Pulmonary
Arterial pressure 120/80 mmHg; 95 mmHg mean 25/10 mmHg; 15 mmHg mean
Capillary pressure 30 mmHg mean 10 mmHg mean
Venous pressure 2-5 mmHg 2-5 mmHg
As consequence the work of the right ventricle in pumping blood is much reduced compared to the work of the left ventricle.
The low intracapillary hydrostatic pressure, a consequence of the low pulmonary arterial pressure, means that normally the osmotic force tending to move fluid into pulmonary capillaries is greater than the hydrostatic pressure moving fluid out.
Pc = capillary hydrostatic pressure
pc = capillary osmotic pressure (due to plasma protein, oncotic pressure)
Pt = tissue hydrostatic pressure
pt = tissue osmotic pressure
Hydrostatic pressure difference (Pc - Pt) tends to move fluid out of capillaries
Osmotic pressure difference (pc - pt) tends to move fluid into capillaries
Also the pulmonary vascular resistance is only about one-sixth to one-ninth of the systemic circulation and low resistance due mainly to less small vessel smooth muscle (arterioles).
The force of gravity affects the distribution of pulmonary blood flow by changing the regional vascular transmural pressure and, consequently, the vascular diameter. This distribution is largely governed by the relationship between blood pressure and vascular pressure and venous pressure can be understood if one considers the lung as a series of "zones".
In the upright posture, pulmonary vascular hydrostatic pressure decreases at increasing heights above the lung because of the effect of gravity. Thus, blood flow is highest in the base of the lungs and decreases toward the apex.
Zone 1: Alveolar air pressure greater than either pulmonary arterial of venous pressures, so vessels collapsed and flow close to zero (Note: does not exist in normal lung, but can occur in pulmonary hypotension)
Zone 2: Alveolar air pressure less than pulmonary arterial pressure but greater than pulmonary venous pressure, so vessels partially collapsed and flow is low
Zone 3: Alveolar air pressure less than both pulmonary arterial and venous pressures, so vessels open for full length and flow highest
In the prone posture, all lung regions are near heart level, so the effect of gravity is much less and the pulmonary flow is more uniform
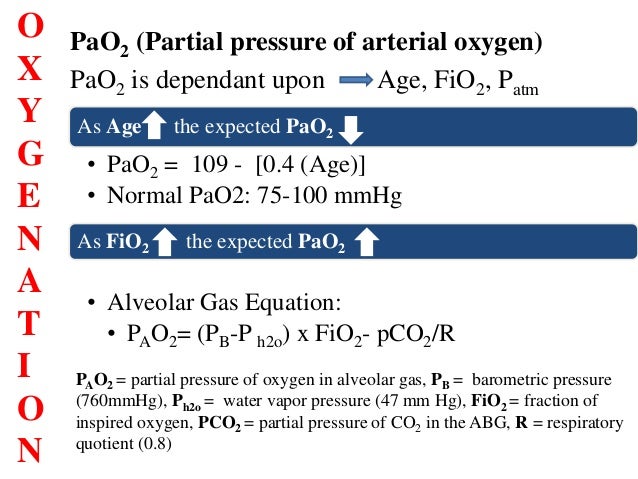
Partial Pressures of O2 and CO2 in the body (normal, resting conditions):
- Alveoli
- PO2 = 100 mm Hg
- PCO2 = 40 mm Hg
- Alveolar capillaries
- Entering the alveolar capillaries
- PO2 = 40 mm Hg (relatively low because this blood has just returned from the systemic circulation and has lost much of its oxygen)
- PCO2 = 45 mm Hg (relatively high because the blood returning from the systemic circulation has picked up carbon dioxide)

paper 2013
While in the alveolar capillaries, the diffusion of gasses occurs: oxygen diffuses from the alveoli into the blood and carbon dioxide from the blood into the alveoli.
- Leaving the alveolar capillaries
- PO2 = 100 mm Hg
- PCO2 = 40 mm Hg
Blood leaving the alveolar capillaries returns to the left atrium and is pumped by the left ventricle into the systemic circulation. This blood travels through arteries and arterioles and into the systemic, or body, capillaries. As blood travels through arteries and arterioles, no gas exchange occurs.
- Entering the systemic capillaries
- PO2 = 100 mm Hg
- PCO2 = 40 mm Hg
- Body cells (resting conditions)
- PO2 = 40 mm Hg
- PCO2 = 45 mm Hg
Because of the differences in partial pressures of oxygen and carbon dioxide between the systemic capillaries and the body cells, oxygen diffuses from the blood and into the cells, while carbon dioxide diffuses from the cells into the blood.
- Leaving the systemic capillaries
- PO2 = 40 mm Hg
- PCO2 = 45 mm Hg
Blood leaving the systemic capillaries returns to the heart (right atrium) via venules and veins (and no gas exchange occurs while blood is in venules and veins). This blood is then pumped to the lungs (and the alveolar capillaries) by the right ventricle.
C. GAS TRANPORT : movement of gases within the pulmonary capillaries through the circulation to the peripheral capillaries in the organs, and then a movement of gases back to the lungs along the same circulatory route.
Oxygen transport
Hemoglobin (Hb), an intracellular protein contained in erythrocytes, is the primary vehicle for transporting oxygen in the blood (98.5 ). Oxygen is also dissolved in plasma ,but to a much lesser degree (1.5).
Under certain conditions, oxygen bound to the hemoglobin is released into the body tissue, and under others, it is absorbed from the tissue into the blood. Each hemoglobin molecule has a limited capacity for holding oxygen molecules. How much of that capacity that is filled by oxygen bound to the hemoglobin at any time is called the oxygen saturation. Expressed as a percentage, the oxygen saturation is the ratio of the amount of oxygen bound to the hemoglobin, to the oxygen carrying capacity of the hemoglobin. The oxygen carrying capacity is determined by the amount of hemoglobin present in the blood.
The amount of oxygen bound to the hemoglobin at any time is related, in large part, to the partial pressure of oxygen to which the hemoglobin is exposed. In the lungs, at the alveolar-capillary interface, the partial pressure of oxygen is typically high, and therefore the oxygen binds readily to hemoglobin that is present. As the blood circulates to other body tissue in which the partial pressure of oxygen is less, the hemoglobin releases the oxygen into the tissue because the hemoglobin cannot maintain its full bound capacity of oxygen in the presence of lower oxygen partial pressures.

which the partial pressure of oxygen is less, the hemoglobin releases the oxygen into the tissue because the hemoglobin cannot maintain its full bound capacity of oxygen in the presence of lower oxygen
Why is the partial oxygen pressure of human tissues a crucial parameter? Small molecules and hypoxia - Carreau - 2011 - Journal of Cellular and Molecular Medicine
Kidney local pO 2
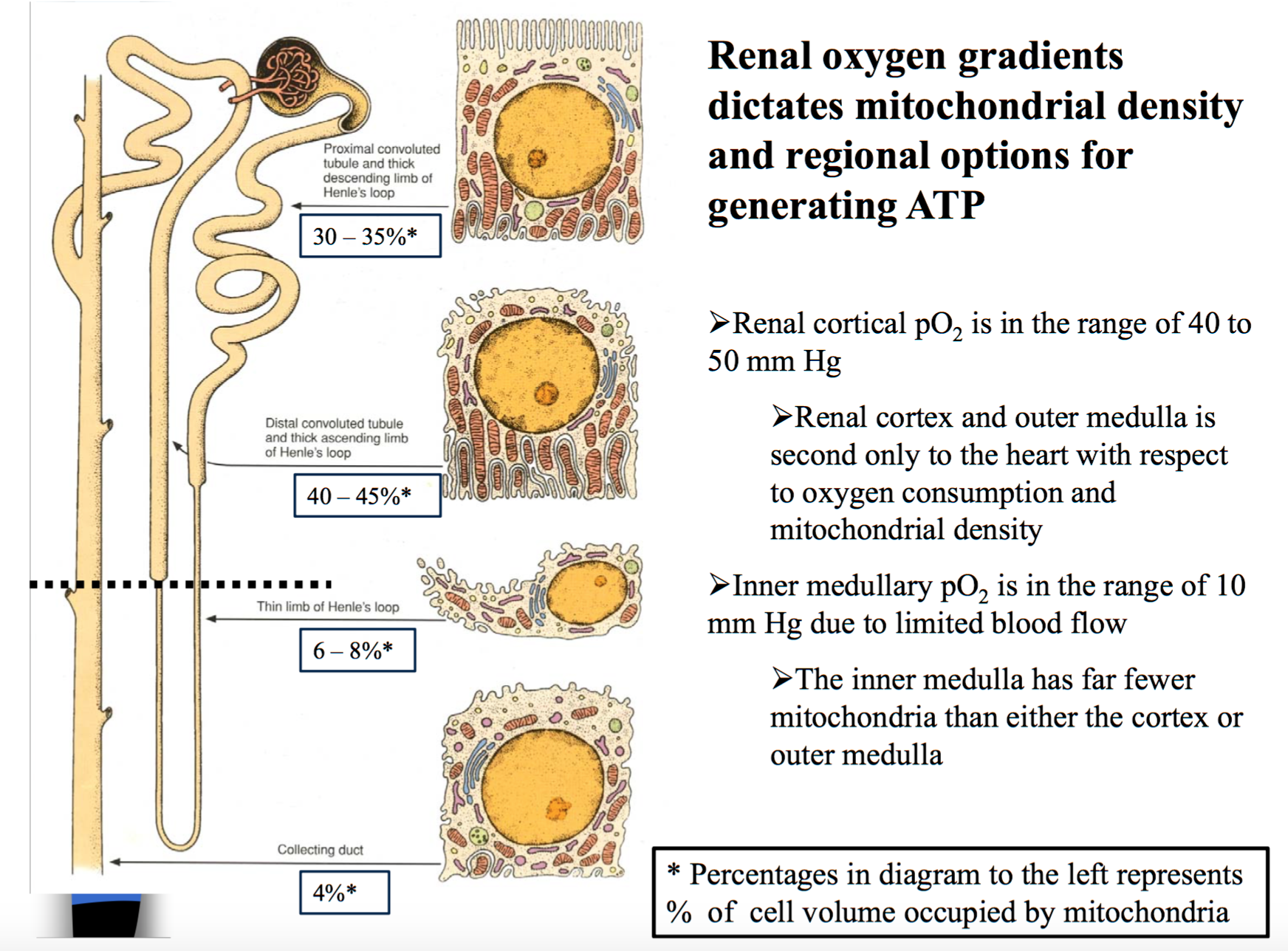
Kidney Biochemistry
Rhythmic Oxygen Levels Reset Circadian Clocks through HIF1α: Cell Metabolism(16)30499-5
Day/night pattern of arterial blood gases in the cow - ScienceDirect
Skin physioxia: oxygen partial pressure in normal skin and cutaneous...

Why is the partial oxygen pressure of human tissues a crucial parameter? Small molecules and hypoxia
Oxygen partial pressure in outer layers of skin: simulation using three-dimensional multilayered models.
Oxygen partial pressure in outer layers of skin of human finger nail folds fulltext

Circadian patterns in men acclimatized to intermittent hypoxia, 2001
Primitivo: Gas Exchange: Diffusion & Partial Pressure Gradients - Video & Lesson Transcript | Study.com