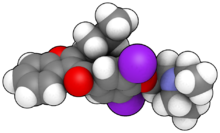
AMIODARONE a potent class III anti-arrhythmic drug, is a iodine-rich compound with a structural resemblance to thyroid hormones triiodothyronine (T3) and thyroxine (T4).

It is used for the treatment of tachyarrhythmias, paroxysmal supraventricular tachycardia, atrial fibrillation, flutter and, to a lesser extent, of ischemic heart disease.
It:
- prolongs phase 3 of the cardiac action potential
- shows beta blocker-like and potassium channel effects
- slows intracardiac conduction via sodium-channel effects.

INDICATION FOR USE:
-Ventricular fibrillation
-Ventricular tachycardia
-Atrial fibrillation

PHARMACOLOGY OF AMIODARONE:
Amiodarone is a benzofuranic derivative whose structural formula closely resembles that of T4. It contains approximately 37% iodine by weight, in particular iodine 37,2 mg for 100 mg of active substance. Considering that the optimal daily iodine intake is 150-200 ug, amiodarone treatment releases 50 to 100 fold excess iodine daily. Moreover, amiodarone is distributed in several tissues, including adipose tissue, liver, lung and, to a lesser extent, kidneys, heart, skeletal muscle, thyroid and brain, from which it is slowly released, so amiodarone’s tissue T/2 is about 2 months.
Amiodarone is metabolized through different pathways, the most important being dealkylation, which leads to formation of DEA. Approximately 6-75% of amiodarone is eliminated through bile and feces.

AMIODARONE'S EFFECT ON THYROID
In peripheral tissues, particularly the liver, amiodarone inhibits type 5’deiodinase activity, which normally removes an atom of iodine from the outer ring of T4 to convert it in T3.
This inhibition may persist for several months after amiodarone withdrawal.
- Apparently amiodarone does not affect the distribution and fractional removal of T3 from the plasma pool. In addition,
- the drug inhibits thyroid hormone entry into peripheral tissues.
Both mechanisms contribute to
- the increased serum T4 concentration and the
- decreased serum T3 concentration in euthyroid subjects given long-term amiodarone therapy.
Amiodarone administration is also associated dose- and time dependent changes in serum TSH concentration. With a daily dose of 200-400 mg of the drug, serum TSH levels are usually normal, although an increased TSH response to intravenous TRH administration is frequently observed. With higher dose of the drug, an increase in serum of TSH concentration may occur during the early months of treatment, but this is generally followed by a return to normal. Amiodarone may also directly affects TSH synthesis and secretion at the pituitary level. The increased serum TSH concentration may also result from the inhibition of type II 5’-deiodinase which converts T4 to T3 in the pituitary, by either amiodarone or desethylamiodarone.
The effect of Amiodarone on thyroid.2001
THYROID CITOTOXICITY:
Chiovato reported that amiodarone had a cytotoxic effect on thyroid cells, although is occurred at a lower molar concentration in freshly prepared human follicles, which trap and organify iodide, than in rat FRTL-5 cells, which have an active iodide pump but are inable to organify iodide.
In human thyroid follicles, lysis of 50% of thyroid cells occurred at concentration of amiodarone (about 200 umol/l) much lower than potassium iodide.
Moreover, amiodarone cytotoxicity was also shows in Chinese hamster ovary cells, a non-thyroid cells line.
DEA, the main amiodarone metabolite, is even more cytotoxic for thyroid cells than amiodarone, and its intrathyroidal concentration is higher than that of the parental drug.
It has been shown recently that in thyroid cells iodide excess induced apoptosis through a P53-independent mechanism involving oxidative stress and associated with production of reactive oxygen species and a marked increase in lipid peroxide levels.
Finally, it is unclear whether non-thyroid amiodarone-induced abnormalities are more common in patients with amiodarone thyroid toxicity.
In the rat, it was shown that amiodarone administration is associated with ultrastructural changes indicative of thyroid cytotoxicity, which were distinct from those induced by excess iodine alone.
These included marked distortion of thyroid architecture, apoptosis, necrosis, included bodies, lipofuscinogenesis, macrophage infiltration, and markedly dilated endoplasmic reticulum. The latter findings might be compatible with the disruption of protein sorting pathways leading to a drug-induced form of endoplasmic reticulum storage disease.
The fact that amiodarone, being amphiphilic, strongly binds to intralysosomial phospholipids, making them indigestible by phospholipases, may contribute to these subcellular changes.
Similar subcellular abnormalities are been observed during amiodarone treatment in other organs, such as liver, lung, heart, skin, cornea, and in peripheral nerves fibers and blood leukocytes. Accumulation of amiodarone in the different tissues and he long terminal half-life of amiodarone and its metabolites represent important factors of the occurrence of the above changes.
AMIODARONE-INDUCED THYROID DISFUNCTION:
Although the majority of patients given amiodarone remain euthyroid, some develop thyroid dysfunction, thyrotoxicosis and hypothyroidism.
Amiodarone-induced thyrotoxicosis (AIT) appears to occur more frequently in geographical areas with low iodine intake, whereas AIH is more frequent in iodine-sufficient areas. In particular, in a study carried out simultaneously in Wester Tuscany (moderately low iodine intake) and Massachusetts (normal iodine intake) it is was found that the incidence of AIT was about 10% in Italy and 2% in USA, while incidence of AIH was 5% in Italy and 5% in USA.

Two studies have prospectively evaluated the incidence of amiodarone-induced dysfunction:
•in a study of 58 consecutive euthyroid patients residing in a Dutch region with moderately sufficient iodine intake, AIT occurred in 12,1% of cases and AIH in 6,9%.
•In a prospective study carried out in a moderately iodine-deficient Italian area, AIT occurred in 2 of 13 patients (15%) and AIH in 5 of 7 patients (71%) who had evidence of Hashimoto’s thyroiditis before treatment.
A high prevalence of thyroid dysfunction was recently reported in an iodine-deficient area (Sardinia, Italy) in a young adult population with β-thalassemia mayor who received amiodarone therapy. Five of 22 patients (23%) developed overt hypothyroidism, compared with 3 of 73 (4%) control β-thalassemic patients not receiving amiodarone therapy, and 3 amiodarone treated patients (14%) developed AIT (2 overt, one subclinical).
In the case of β-thalassemia, thyroid damage related to increased intrathyroidal iron deposits probably contributed to the high rate of amiodarone-associated thyroid dysfunction, particularly hypothyroidism.


In general, the various published studies reported an overall incidence of AIT ranging from 1% to 23% and of AIT I ranging from 1% to 32%. Thus, irrespective of iodine intake, it may be estimated that the overall incidence of amiodarone-induced thyroid dysfunction be between 2% and 24%, most commonly in the range of 14%-18%.
It is worth mentioning that in one study the addition of phenytoin to amiodarone was associated with a 49% incidence of thyroid dysfunction after a prolonged follow-up.
Like-wise, evaluation of a large series of adults with congenital heart disease revealed a prevalence of thyroid dysfunction in 36% of patients: female sex, complex cyanotic heart disease, previous Fontain-type surgery, and a amiodarone-associated thyroid dysfunction.
AMIODARONE-INDUCED THYROTOXICOSIS (AIT):
AIT may develop, often suddenly and explosively, early or after many years of amiodarone treatment.
An interesting feature of AIT is that, due to tissue storage of drug and its metabolites and to their slow release, the effect of amiodarone can persist for a long period of time. The daily or cumulative dose of amiodarone does not seem to be relevant for the occurrence of AIT. There are not parameters allowing predictability of AIT, although it has been suggested that the baseline lack of a TSH response to TRH may represent a risk factor for the subsequence occurrence of AIT. A relative predominance of AIT among men, with a M:F ratio of 3:1, has been reported.
Pathogenesis
The pathogenesis of AIT is complex and not completely understood. The disease may develop both in a normal thyroid gland or in a gland with preexisting abnormalities.
In a study in a moderately iodine-deficient area, diffuse goiter was found in 29% of AIT, and nodular goiter occurred in 38%, but the thyroid was apparently normal in the remaining 33% of cases.
The occurrence of AIT is also reported in studies from iodine-sufficient areas.
Humoral thyroid autoimmunity seems to play little, if any, role in the development of AIT in patients without underlying thyroid disorders. Circulating antithyroglobulin, antithyroid peroxidase, , and TSH receptors (TRAb) antibodies were found only in AIT patients with preexisting thyroid abnormalities (mostly diffuse goiter), but not in those with apparently normal thyroid glands.
A possible pathogenetic hypothesis suggests that AIT is due to excessive thyroid hormone synthesis induced by the iodine load. Intrathyroidal iodine content, assessed by x-ray fluorescence, was found to be markedly increased in AIT patients, irrespective of the presence of an intrinsic thyroid abnormality.
The perchlorate discharge test is negative, indicating that there is no relevant impairment of iodine organification. Interestingly, a normalization of intrathyroidal iodine content has been reported after the restoration of euthyroidism in AIT patients.
In patients with preexisting thyroid abnormalities (diffuse or nodular goiter, latent Graves’ disease) the 24-h thyroid radioactive iodine uptake (RAIU) values were in some cases higher than 8% (and as high as 64%) despite the iodine load, although in iodine-sufficient area such as the USA, the RAIU is almost always very low.
This suggests that in patients with an underlying thyroid disorders and residing in a mildly iodine-deficient area, the thyroid gland may fail to adapt normally to excess iodine load, resulting in a inappropriately elevated RAIU values despite the presence of excess plasma iodine.
This subgroup of AIT patients usually have normal or slightly elevated serum interleukin-6 levels.
This cytokine is a good marker of thyroid-destructive processes and, therefore, increased in circulation after radioiodine therapy, intranodular ethanol injection, and fine needle aspiration.
An increased IL-6 concentration is also found in subacute thyroiditis. The fact that serum IL-6 levels are normal or slightly increased in this subgroup of AIT patients suggests that thyroid destruction processes do not represent an important pathogenetic mechanism in most of these cases. This form of AIT with an underlying thyroid abnormality, normal/elevated RAIU values but low values in iodine sufficient regions, and normal/elevated serum IL-6 levels, has been defined type I AIT.
Further support to the concept type I AIT is due to excess iodine-associated excessive thyroid hormone synthesis comes from the observation that these patients have color flow Doppler sonography (CFDS) patterns that indicate a hyperfunctioning gland with hipervascularity, as seen in spontaneous hyperthyroidism.
These patients usually have no detectable thyroid abnormalities on physical examination or ultrasonography, although in some cases there may be a small, tender goiter, and thyroid autoantibody tests are negative. In addition they have very low (usually <2-3%) RAIU values.
Serum IL-6 concentration are usually markedly elevated and absence of hypervascularity is observed on CFDS.
Both the above features are typically encountered in thyroid-destructive processes, such as subacute thyroiditis. Further support to the concept that this form of AIT, defined as type II, is related to a thyroid-destructive process is provided by the hystopathological examination of the thyroids of few patients.
While euthyroid amiodarone-treated patients showed minimal or no evidence of thyroid follicular damage, the glands of two patients with AIT showed moderate to severe follicular damage and disruption.
Other small surgical series showed signs of thyroid damage, with swelling of follicular cells, vacuolization of the cytoplasm, and fibrosis.
Therefore, type II AIT appears to be a form of destructive thyroiditis with associated leakage of preformed hormones from damaged follicles. This is in keeping with the in vitro studies demonstrating the cytotoxic effect of amiodarone and its metabolites.
Further support comes from the observation that in this subgroup of AIT patients, the thyrotoxic phase is sometimes followed by mild hypothyroidism, as may happen after subacute thyroiditis. This progression may be accelerated by re-exposure of the patient to an iodine load.
The relative prevalence of the two form of AIT is unknown, but it may depend on the ambient iodine intake.
SIDE EFFECTS:
Clinical manifestations of thyrotoxicosis
Classical symptoms of thyrotoxicosis may be absent, due to the antiadrenergic action of amiodarone and its impairment of conversion of T4 to T3; goiter may be present or absent, with or without pain in the thyroid region: ophthalmopathy is usually absent, unless AIT occurs in a patient with Grave’s disease.
AIT may be heralded by a worsening of the underlying cardiac disorders, with tachyarrythmias or angina.
Diagnosis of AIT may be a difficult challenge in patients with severe non nonthyroidal illness, because the latter may dominate the clinical picture and result in increased serum free T4, decreased/suppressed serum TSH, and decreased serum total and free T3 concentrations: under these circumstances, measurement of serum free T3 concentration may be useful in establishing the diagnosis.
Serum thyroglobulin is often increased in AIT, but this may not represent a good marker of thyroid destruction in goitrous patients. In addition, unexplained suppression of serum thyroglobulin secretion has been reported in a few AIT patients.
Serum sex hormone binding globulin (SHBG) concentration is elevated in AIT patients but not in euthyroid amiodarone-treated subjects with hyperthyroxinemia; however, this assay is of limited importance in individual patients, due to numerous factors affecting serum SHBG levels.
Clinical manifestation in thyrotoxicosis are mainly cardiovascular symptoms.
•Elevation of heart rate
•Elevation of myocardial contractility
•Elevation of stroke volume
•Elevation of myocardial oxygen consumption
•Elevation of systolic blood pressure
•Reduction of systemic vascular resistance
•Reduction of diastolic blood pressure
The most common cardiac complication are arrhythmias (mainly atrial fibrillation), heart failure and hypertension.
Cardiovascular manifestations of thyrotoxicosis and thyroid dysfunction caused by amiodarone.2004
TREATMENT:
Treatment of AIT is a mayor challenge. The high intrathyroidal iodine content reduces the effectiveness of conventional thionamide drug therapy. The generally low or suppressed RAIU values makes the administration of radioiodine therapy not feasible. An increase in RAIU values has been reported after administration of exogenous TSH.The possibility should be revaluated using recombinant human TSH.
Thyroidectomy may represent a valid option for AIT patients resistant to medical treatment, although the underlying cardiac condition and thyrotoxic state may increase the surgical risk or even exclude surgery in some patients. About 30 patients treated by thyroidectomy have been reported: this procedure was associated with a prompt control of thyrotoxicosis, and no death occurred. Plasmapheresis, aimed at removing the excess thyroid hormone from the circulation, has been reported to be efficacious, but this is usually transient and followed by an exacerbation of AIT.

The identification of the different subtypes of AIT may provide a rational bases for the choice of the appropriate medical treatment in an effort to improve the therapeutic outcome.
In type I AIT the goal of treatment should be, on one hand, to block the further organification of iodine and synthesis of thyroid hormones.
Since the iodine-rich thyroid is more resistant to the therapeutic efficacy of the thionamides, larger than usual daily doses of methimazole (40-60 mg) or propylthiouracil (600-800 mg) are often necessary.
On the other hand, one should also decrease the entrance of iodine into the thyroid and deplete intrathyroidal iodine stores to improve the therapeutic efficacy of thionamides and to allow subsequent radioiodine therapy. The latter effect can be achieved by potassium perchlorate, a drug that inhibits thyroid iodine uptake.
Treatment of AIT by the simultaneous administration of potassium perchlorate and methimazole was reported in a study with 23 patients. These were treated with methimazole (40 mg daily) alone, with methimazole and potassium perchlorate (1 g daily), or were not treated.
Only the combined treatment controlled thyrotoxicosis in all cases. In addition, the time required for the attainment of euthyroidism was shorter than that in patients responsive to conventional thionamide treatment.
The combined treatment was associated with a transient rise in serum thyroid hormone levels and urinary iodine excretion. These result were subsequently confirmed by other studies.
The limitation of potassium perchlorate is its toxicity, particularly agranulocytosis and aplastic anemia, and renal side effect.
Thionamides with or without potassium perchlorate are not an appropriate form of therapy for type II AIT, which is a detructive thyroiditis induced by amiodarone.
Steroids are a good and effective therapeutic approach in these cases because of their membrane-stabilizing and anti-inflammatory effects. In addition, they are beneficial because of their inhibition of 5’-D activity. Steroids have been employed in AIT at different doses (50-80 mg prednisone or 3-6 mg dexamethasone daily) and different time schedules (7-12 weeks). Results of steroid treatment, either alone or in combination with antithyroid drugs or plasmapheresis, have been favorable in most studies in patients with type II AIT.
A relevant problem is whether amiodarone therapy should be continued or not. Obviously, amiodarone is a very effective drug for the underlying cardiac problem, and quite often these patients are resistant to other antiarrhythmic drugs.
In addition, even discontinuation of amiodarone therapy does not prevent a continuing effect on the thyroid due to its long half-life. Furthermore, in view of the hypothyroid-like effect of amiodarone and its metabolites on the heart, amiodarone might, to some extent, paradoxically protect the heart from thyroid hormone excess; therefore, withdrawal of the drug might be associated with an exacerbation of “heart thyrotoxicosis”.
Indeed, a worsening of thyrotoxic symptoms ad cardiac conditions has occasionally been reported after amiodarone was discontinued.
There are a few reports in the literature demonstrating successful management of AIT with antithyroid drugs while amiodarone therapy was continued.
Since AIT is widely accepted to be much more difficult to treat than “normal” hyperthyroidism, is supposed that withdrawal of amiodarone, when feasible as in the case of non-life-threatening arrhythmias, should be part of management of AIT patients, although some patients have mild disease and respond to thionamide and/or glucocorticoid therapy, depending upon the type of AIT. In these patients amiodarone may be continued since the AIT seems to be self-limited.
A rational approach might be the following:
1)Identify the subtype of AIT if possible
2)Treat type II with steroids for 3 months, with a starting dose of 30-40 mg prednisone (or equivalent) and a gradual, slow reduction to minimize the risk of recurrences
3)Treat type I AIT with methimazole and potassium perchlorate (1 g daily for no more than 30-40 days)
4)If the two types cannot be distinguished (mixed forms), triple therapy with a thionamide, potassium perchlorate, and glucorticoids is a pratical solution.
Preparation with iopanoic acid rapidly controls thyrotoxicosis in patients with amiodarone-induced thyrotoxicosis before thyroidectomy.2002...
In cases in which withdrawal of amiodarone is not feasible and medical therapy has failed, thyroidectomy represents a useful alternative. Definitive treatment of the underlying thyroid disorder will usually be required in most type I AIT patients; this can occasionally be accomplished by radioiodine, provided the RAIU values become adequate. Most type II patients will remaine euthyroid after resolution of the thyrotoxicosis; some of them may eventually develop hypothyroidism, either spontaneously or after reexposure to iodine. The hypothyroidism that occasionally occurs after postpartum lymphocytic thyroiditis or painful, subacute thyroiditis since the excess iodine and amiodarone is discontinued. In patients with a history of AIT in whom amiodarone becomes necessary after it has been discontinued, ablation of the thyroid with radioiodine before resuming amiodarone should be strongly considered.
CASE REPORTS:
