DESCRIPTION
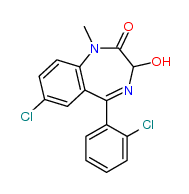
A benzodiazepine is a psychoactive drug whose core chemical structure is the fusion of a benzene ring and a diazepine ring. The first benzodiazepine, chlordiazepoxide (Librium), was discovered accidentally by Leo Sternbach in 1955, and made available in 1960 by Hoffmann–La Roche, which has also marketed diazepam (Valium) since 1963.
Benzodiazepines enhance the effect of the neurotransmitter gamma-aminobutyric acid, which results in sedative, hypnotic (sleep-inducing), anxiolytic (anti-anxiety), anticonvulsant, muscle relaxant and amnesic action. These properties make benzodiazepines useful in treating anxiety, insomnia, agitation, seizures, muscle spasms, alcohol withdrawal and as a premedication for medical or dental procedures. Benzodiazepines are categorized as either short-, intermediate- or long-acting. Short- and intermediate-acting benzodiazepines are preferred for the treatment of insomnia; longer-acting benzodiazepines are recommended for the treatment of anxiety.

CLASSIFICATION
- Benzodiazepine family
- BB
INDICATIONS
PHARMACOKINETICS
A benzodiazepine can be placed into one of three groups by its elimination half-life, or time it takes for the body to eliminate half of the dose.
- Short-acting compounds have a half-life of 1–8 hours. They have few residual effects if taken before bedtime, rebound insomnia may occur upon discontinuation and they might cause day time withdrawal symptoms such as next day rebound anxiety with prolonged usage. Examples are brotizolam, midazolam and triazolam.
 Triazolam
Triazolam
- Intermediate-acting compounds have a half-life of 8–40 hours. They may have some residual effects in the first half of the day if used as a hypnotic. Rebound insomnia, however, is more common upon discontinuation of intermediate-acting benzodiazepines than longer acting benzodiazepines. Examples are estazolam, flunitrazepam, lormetazepam, nitrazepam and temazepam.
 Lormetazepam
Lormetazepam
- Long-acting compounds have a half-life of 40–200 hours. They have a risk of accumulation in the elderly and in individuals with severely impaired liver function, but they have a reduced severity of rebound effects and withdrawal. Examples are diazepam and chlordiazepoxide.
 Diazepam
Diazepam
Some benzodiazepines have long-acting active metabolites such as diazepam and chlordiazepoxide, which are metabolised into desmethyldiazepam. Desmethyldiazepam has a half-life of 36–200 hours.

MOLECULAR MECHANISM
Benzodiazepines work by increasing the efficiency of a natural brain chemical, GABA, to decrease the excitability of certain types of brain cells called neurons. This reduces the communication between neurons and therefore has a calming effect on many of the functions of the brain.
The subset of GABAA receptors that also bind benzodiazepines are referred to as benzodiazepine receptors (BzR). The GABAA receptor is a heteromer composed of five subunits, most commonly two α's, two β's and one γ (α2β2γ). For each subunit, many subtypes exist (α1-6, β1-3 and γ1-3). GABAA receptors that are made up of different combinations of subunit subtypes have different properties, different distributions in the brain and different activities relative to pharmacological and clinical effects. Benzodiazepines bind at the interface of the α and γ subunits on the GABAA receptor. Binding also requires that alpha subunits contain a histidine amino acid residue, (i.e., α1, α2, α3 and α5 containing GABAA receptors). For this reason, benzodiazepines show no affinity for GABAA receptors containing α4 and α6 subunits with an arginine instead of a histidine residue.


Once bound to the benzodiazepine receptor, the benzodiazepine ligand locks the benzodiazepine receptor into a conformation in which it has a greater affinity for the GABA neurotransmitter. This increases the frequency of the opening of the associated chloride ion channel and hyperpolarizes the membrane of the associated neuron. The inhibitory effect of the available GABA is potentiated, leading to sedatory and anxiolytic effects. Furthermore, different benzodiazepines can have different affinities for BzRs made up of different collection of subunits. For instance, those with high activity at the α1 are associated with stronger hypnotic effects, whereas those with higher affinity for GABAA receptors containing α2 and/or α3 subunits have good anti-anxiety activity.

The benzodiazepine class of drugs also interact with peripheral benzodiazepine receptors. Peripheral benzodiazepine receptors are present in peripheral nervous system tissues, glial cells and to a lesser extent the central nervous system. These peripheral receptors are not structurally related nor coupled to GABAA receptors. They modulate the immune system and are involved in the body response to injury. Benzodiazepines also function as weak adenosine reuptake inhibitors. It has been suggested that some of their anticonvulsant, anxiolytic and muscle relaxant effects may be in part mediated by this action.

PHARMACOGENOMICS
SIDE EFFECTS
TOXICITY
RESISTANCE
DEPENDENCE AND WITHDRAW
BENZODIAZEPINES: HOW THEY WORK AND HOW TO WITHDRAW