DEFINITION
Seasonal affective disorder is a mood disorder in which people who have normal mental health throughout most of the year experience episodes of major depression that tend to recur during specific times of the year, usually in winter. For those people the shortening of the day, the decreasing amounts of sunlight, bring with them a debilitating package of hibernation-like symptoms that can last from the beginning of September to the end of May every year.
PATHOGENESIS
" It is chiefly the changes of the seasons that produces diseases " Hippocrates, more than 2000 years ago.
The biology that underlies the association between seasonality and mood disorders is still controversial. Various proximate causes have been proposed:
A lack of serotonin that can be due to reduced sunlight.

The activity of serotonin arises in the brainstem from clusters of neurons known as the raphe nucleus . From the brain, serotonin neurons extend to virtually all parts of the central nervous system. Serotonin action is based on the activation of its receptors 5-HT . The serotonin receptors,(5-hydroxytryptamine receptors) , are a group of G protein-coupled receptors (GPCRs) and ligand-gated ion channels (LGICs).
Family Type Mechanism Potential
5-HT1 Gi/Go-protein coupled - Decreasing cellular levels of cAMP - Inhibitory
5-HT2 Gq/G11-protein coupled - Increasing cellular levels of IP3 and DAG - Excitatory
5-HT3 Ligand-gated Na+ and K+ cation channel - Depolarizing plasma membrane -Excitatory
5-HT4 Gs-protein coupled - Increasing cellular levels of cAMP - Excitatory
5-HT5 Gi/Go-protein coupled - Decreasing cellular levels of cAMP - Inhibitory
5-HT6 Gs-protein coupled - Increasing cellular levels of cAMP - Excitatory
5-HT7 Gs-protein coupled - Increasing cellular levels of cAMP - Excitatory
Especially 5-HT1, 5-HT2, 5-HT4, 5-HT6 E 5-HT7 have a role in the regulation of mood.
The role of serotonin in SAD is supported by the fact that many patients respond well to selective serotonin re-uptake inhibitors SSRI
The acute increases in the amount of synaptic monoamines produce secondary neuroplastic changes: the serotonin 5-HT1B receptor interacts with a calcium-binding protein named p11 and the brain-specific transgenic overexpression of p11 produced an antidepressant phenotype, implicating this SSRI-mediated upregulation of p11 as an important mechanism downstream of serotonin receptor activation.
 As the image shows, depressive states are characterized notably by a decrease of BDNF and p11 levels. In the hippocampus, antidepressant treatment increases the expression of BDNF which in turn, upregulates p11 level. The increase in p11 promotes the availability of 5-HT1BR at the plasma membrane. It also enhances BDNF levels through a positive regulation loop involving tPA/plasminogen activity
As the image shows, depressive states are characterized notably by a decrease of BDNF and p11 levels. In the hippocampus, antidepressant treatment increases the expression of BDNF which in turn, upregulates p11 level. The increase in p11 promotes the availability of 5-HT1BR at the plasma membrane. It also enhances BDNF levels through a positive regulation loop involving tPA/plasminogen activity
Chronically administered antidepressants have also been shown to upregulate the transcription factor CREB (cyclic-AMP-response-element-binding protein), which is downstream of several serotonin and other stimulatory G-protein-coupled receptors, in the hippocampus. 
Activation of the cyclase increases the cAMP concentration and induces activation of the cyclic AMP-dependent protein kinase A ( PKA ). Activation of PKA can phosphorylate and covalently modify a number of target proteins. PKA translocate to the nucleus where it phosphorylates the cyclic AMP response element binding proteins ( CREBs ). Phosphorylation by ERK of the repressor isoform CREB-2 removes its inhibition on CREB-1a. Phosphorylation of CREB-1a induces transcription of early/late genes containing cyclic AMP response elements, leading to growth of new synaptic connections and potentially transmitter release.
The molecular neurobiology of depression, 2008
Moreover, mice incapable of turning serotonin into N-acetylserotonin (by serotonin N-acetyltransferase) appear to express "depression-like" behavior, and antidepressants such as fluoxetine increase the amount of the enzyme serotonin N-acetyltransferase, resulting in an antidepressant-like effect.

Melatonin is centrally involved in the development of SAD.
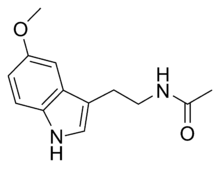
Melatonin is produced in the pineal gland. The production and secretion of melatonin are mediated largely by postganglionic retinal nerve fibers that pass through the retinohypothalamic tract to the suprachiasmatic nucleus, then to the superior cervical ganglion, and finally to the pineal gland. During daylight hours, the retinal photoreceptor cells are hyperpolarized, which inhibits the release of norepinephrine. The retinohypothalamic–pineal system is quiescent, and little melatonin is secreted. With the onset of darkness, the photoreceptors release norepinephrine, thereby activating α1- and β1 - adrenergic receptors in the gland. The activation of α1- and β1- adrenergic receptors in the pineal gland raises cyclic AMP and calcium concentrations and activates arylalkylamine N-acetyltransferase, initiating the synthesis and release of melatonin.

Now, melatonin, activating its receptors, can cause drowsiness and this could explain the symptom of sleepiness in SAD patients, in which we meet a phase delay of melatonin secretion, as well as changes in its onset, duration and offset.
Two membrane-bound melatonin receptors have been identified: ML1 (a high-affinity receptor) and ML2 (a low-affinity receptor). Activation of ML1 melatonin receptors, which belong to the family of guanosine triphosphate–binding proteins (G protein–coupled receptors),results in the inhibition of adenylate cyclase activity in target cells. These receptors are involved in the regulation of circadian rhythms. The ML2 receptors are coupled to the stimulation of phosphoinositide hydrolysis, but their distribution has not been determined. ML1 has two subtypes, designated Mel1a (or MT1)and Mel1b (or MT2). The MT1 subtype is present in the pars tuberalis of the pituitary gland and the suprachiasmatic nuclei of the hypothalamus. The MT2 subtype is mainly present in the retina.
Melatonin receptor regulates several second messengers: cAMP, cGMP, diacylglycerol, inositol trisphosphate, arachidonic acid, and intracellular Ca2+ concentration ([Ca2+]i). Molecular mechanisms of the melatonin effects involve at least two parallel transduction pathways, one inhibiting adenylyl cyclase (reducing cAMP levels) and the other regulating phospholipide metabolism and [Ca2+] . .
Cellular mechanisms of melatonin action, 1998

The daytime rhythm in serum melatonin concentrations parallels the day–night cycle.
However, a rhythm of about 24 hours' duration also persists in normal subjects kept in continuous darkness. In fact, the circadian rhythm of melatonin secretion is of endogenous origin, reflecting signals originating in the suprachiasmatic nucleus. Environmental lighting does not cause the rhythm but entrains it (alters its timing).
THERAPY
- Light therapy: The later dawn in winter leads to a delay in circadian rhythms and a disconnect between the molecular rhythms of the SCN and the sleep/wake cycle in SAD patients, so that they don’t know when they should sleep or be awake. This hypothesis is largely based on research demonstrating that early morning bright light therapy is the most effective in treating SAD while evening light therapy is often not effective. Therefore, the early morning light is leading to a phase advance in the circadian system putting it back on track with the sleep/wake cycle. In addition, there have been reports that melatonin therapy in the evening can also be effective in producing this same phase advance and may help with the treatment of SAD.
Ain’t no cure for the wintertime blues, 1998
.unito.it/news/1998/981105/full/news981105-8.html
- SSRI (selective serotonin reuptake inhibitor)
- Another potential therapy for depression are melatonin-receptor agonists . MT1 receptors appeared specifically increased in the SCN of depressed patients, and may increase during the course of the disease. These changes may be involved in the circadian disorders and contribute to the efficacy of MT agonists or melatonin in depression.
Alterations of melatonin receptors MT1 and MT2, 2013
Other therapies:
- Carefully timed supplementation of melatonin
- Negative air ionization
- Also physical exercise has shown to be an effective form of depression therapy, particularly when added on in addition to another form of treatment for SAD.