DEFINITION
Alcoholic liver disease. is a term that encompasses the hepatic manifestations of alcohol overconsumption, including steatosis, alcoholic hepatitis and chronic hepatitis, usually associated with hepatic fibrosis or cirrhosis
EPIDEMIOLOGY
Alcohol-related liver disease is one of the most frequent causes of liver damage, associated with high mortality.It represents the major cause of liver diseases in the Western countries and cirrhosis is the fourth cause of death among adult men in the USA. The prevalence of this kind of pathology is strictly related to religious and social traditions of many countries (particularly France, Austria, Germany, Hungary and Spain) and to the relation between the cost of alcoholic beverages and people’s income. Steatosis usually develops in all chronic heavy drinkers, while hepatitis only occurs in 15-20% of people and cirrhosis in about 10-15%.
Women show a higher risk as they tend to hide their addiction rather than men so these pathologies are diagnosed at more advanced stages. Furthermore, they are more susceptible to alcohol-related liver damage (they show a higher risk of developing cirrhosis even after stopping drinking) and they have higher blood levels of ethanol after a standard oral dose, because of the smaller amount of alcohol dehydrogenase in their gastric mucosa.
SYMPTOMS
Steatosis: the patient is usually asymptomatic. Nausea, vomiting and abdominal pain can occur. Two important features are hepatomegaly and anorexia, caused by the prolonged alcohol consumption.
Hepatitis: This state is accompanied by asthenia, anorexia, weight loss and fever, while the liver is increased in size and aches during palpation. Moreover, in 90% of cases, patients show malnutrition, which is also very frequent in the worst states. In such states, the hepatic function can be lost suddenly, following severe episodes of vomiting and diarrhea or an existing infection, such as pneumonia. Typical symptoms of severe alcoholic hepatitis are fever, anorexia, jaundice, hepatomegaly and relapses of vomiting. Sometimes, it is even possible to find signs of hepatic failure like ascites, alcoholic encephalopathy and increased susceptibility to hemorrhages.
Cirrhosis: it can be identified from hepatomegaly, splenomegaly and many other typical clinical features of severe alcohol abusers, like neurological deficiency (loss of memory and ability to concentrate, insomnia, irritability, hallucinations and convulsions) and renal impairment; ascites, portal hypertension and encephalopathy.
DIAGNOSIS
Steatosis: The differential diagnosis with drug-induced or non-alcoholic steatosis demands liver biopsy, which shows large fatty globules in the hepatocyte cytosol due to the accumulation of high quantities of triglycerides. Many times it is possible to identify this condition through laboratory examinations of hepatic enzymes (notably through high blood levels of GOT, GPT and alkaline phosphatase).
Hepatitis: in the mildest cases, diagnosis can be made through biopsy only, where hepatocytes present a swollen and granular appearance, a small-size nucleus and macrovescicular steatosis. However, these states are usually diagnosed through laboratory tests (mostly through high blood levels of GOT,GPT, γGT, bilirubin and reduced albumin and coagulation factors), the evident hepatomegaly and the large number of clinical symptoms.
Cirrhosis: many times, it is diagnosed through the patient's alcohol addiction history, hepatomegaly, splenomegaly and other typical features as ascites and portal hypertension. US, CT and NMR underline these conditions and show the micronodular appearance of cirrhotic liver, while biopsy alone doesn't always allow the recognition of alcoholic etiology.
PATHOGENESIS
Negative effects of chronic intake of alcohol are, on average, caused by ethanol metabolites acetaldehyde and NADH. These derive from the oxidative action of ADH (alcohol dehydrogenase) and MEOS (microsomal ethanol oxidizing system) on ethanol and of ALDH (aldehyde dehydrogenase) on acetaldehyde.
Ethanol metabolism
- Acetaldehyde: it is an extremely toxic and reactive substance whose serum levels are increased in chronic heavy drinkers. Its deleterious effects include impairment of the mitochondrial beta-oxidation of fatty acids, formation of oxygen-derived free radicals (ROS) and depletion of mitochondrial glutathione. In addition, acetaldehyde may bind covalently with several hepatic macromolecules, such as amines and thiols, in cell membranes, enzymes, and microtubules to form acetaldehyde adducts. This binding may trigger an immune response through formation of neoantigens and the following release of inflammatory cytokines, that establish a chronic inflammation of hepatic tissue; an impaired function of intracellular transport through precipitation of intermediate filaments and other cytoskeletal elements; the stimulation of hepatic stellate cells to produce collagen and fibronectin, which slowly leads to fibrosis. It is also responsible for the giant mitochondria (megamitochondria), whose swelling is related to the continuous oxidative damage.
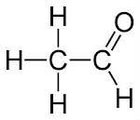
- NADH: the decrease of the NAD+/NADH ratio linked to the oxidation of ethanol and acetaldehyde has many negative effects on hepatocytes. In fact, it causes the increased production of lactate from pyruvate, inducing lactic acidosis; the inhibition of gluconeogenesis accompanied by ketogenesis; the synthesis of fatty acids and triacylglycerol (responsible for “fatty liver”) and the increased plasma levels of VLDL and HDL cholesterol.
In many cases, the different manifestations of alcoholic liver disease occur at the same time, because their pathogenic processes overlap. They share the common hepatocyte injury associated with inflammation and fibrosis. In the worst cases, this condition can evolve into cirrhosis or even hepatocellular carcinoma.

Mechanism of ethanol induced hepatic injury.1990
STEATOHEPATITIS
The prolonged acetaldehyde-related oxidative stress, with peroxidation of lipids and membrane damage, and the depletion of antioxidant molecules induce a condition of acute inflammation of the hepatic tissue, which is aggravated by increased production of the proinflammatory cytokines tumor necrosis factor-alpha and interleukin 6 in the Kupffer cells. These are activated by the products of lipid peroxidation as well as by endotoxin LPS. In fact, ethanol increases the permeability of enteric barrier so that many toxins and bacterial LPS reach liver, binding LBP. This complex is recognised by toll-like receptor-4 (TLR4) on Kupffer cells membrane, inducing by intracellular signalling with MAP kinasi-erb/2 and NFkB the synthesis of TNF-α, which leads hepatocites to necrosis. Furthermore, ROS cause the activation of caspases and the progression towards apoptosis.
Besides, large fatty globules appear in the hepatocyte cytosol as a result of the accumulation of high quantities of triglycerides. This phenomenon is due to many factors:
- the reduced fatty acid oxidation, because of NAD depletion (although, some of the excess NADH may be reoxidized in the conversion of pyruvate to lactate) and the down-regulation of transcriptional factor PPAR alpha, that regulates the expression of genes for catabolic lipid enzymes;
- the increased synthesis of triglycerides, related to the augmented expression of fatty acid synthetase due to the transcription factor SREBP1;
-the reduced secretion, caused by citoskeletal damage on hepatocytes and the poor synthesis of apolipoproteinB.
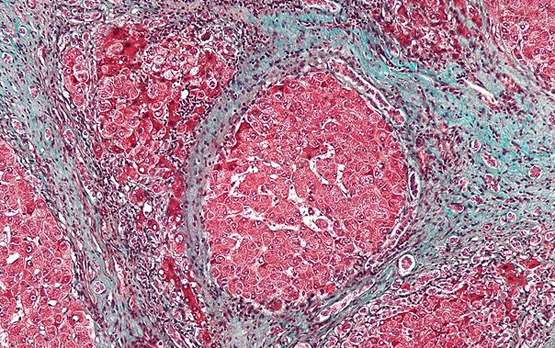
Accordingly, the intracellular concentration of free fatty acids may become high enough to injure membranes, thereby contributing to necrosis, inflammation, and progression to fibrosis and cirrhosis. In fact, a reticular deposition of collagen takes place around the sinusoids, mostly in zone 2 or 3 of the hepatic lobule. The presence of collagen fibers in the Space of Disse prevents exchanges between plasma and the hepatocyte membrane and contributes in causing portal hypertension and ascites. This condition called fibrosis (which can prelude cirrhosis) results from the conversion of the Ito cells into fibroblasts, producing type 13 collagen in response to cellular necrosis, hypoxia and to the release of some inflammatory cytokines as TGFß. Acetaldehyde-induced TGFß promotes the expression of collagen genes and inhibits the action of metalloproteinases: it also stimulates the release of TNF alpha, responsible for the further hepatocyte apoptosis.


Cytokines in alcoholic liver disease.2012
CIRRHOSIS
It is the late stage of many liver diseases and it is characterized by chronic inflammation, fibrosis, hepatocyte necrosis and hepatic failure. Steatosis can be present at varying degrees, but it seems reduced by the progression of fibrosis and necrosis. The main feature is the development of scar tissue that replaces normal parenchyma, blocking the portal flow of blood through the organ and disturbing normal function. Fibrosis consists, in fact, into an alteration in the normally balanced processes of extracellular matrix production and degradation. Damage to the hepatic parenchyma leads to activation of the stellate cells, which become contractile (called myofibroblast) and obstruct blood flow in the circulation. In addition, they secrete TGF-β, which leads to a fibrotic response and proliferation of connective tissue, and TIMP 1 and 2, naturally occurring inhibitors of matrix metalloproteinases, which prevents them from breaking down fibrotic material in the extracellular matrix. Some fibrous tissue bands (septa) separate hepatocyte nodules, which eventually replace the entire liver architecture.

PATIENT RISK FACTORS
Not all alcohol abusers develop hepatic damage. It is known, in fact, that some people have a greater tendency to be affected by this kind of diseases, but the reasons are still unknown. The main factors which influence the development of these conditions are:
- Genetic: there’s great variability in the rate of alcohol metabolism among the population related to genetic polymorphisms of the two main enzymatic systems which oxidize ethanol, the microsomal ethanol oxidizing system (MEOS) and the alcohol dehydrogenase (ADH). The most evident example is given by certain ethnic groups, such as Asians or Native Americans, who are extremely sensitive to ethanol consumption because of the presence of an alcohol dehydrogenase variant with a higher rate of activity, or the deficiency of an isozyme of aldehyde dehydrogenase. These are responsible for the higher acetaldehyde steady-state in blood and for the resulting effects on behaviour;
- Acquired: alcohol-related liver damage seems to be greater in the subjects who are positive to HBV or HCV markers as a result of viral infections. These conditions can act as cofactors in the pathogenic process because those virus are responsible for chronic infections, increasing the hepatic degeneration and the risk of hepatocellular carcinoma;
- Habits:
The amount of ethanol consumption: 60-80 g per day (about 75-100 ml per day) is considered the maximum amount, over that, the risk of liver damage is greatly increased for the majority of the population;
The length of consumption: it has been demonstrated that the chronic intake for 20 years or more of moderate quantities of alcohol showed a higher risk of cirrhosis than that of a 5-year consumption of about 160g per day. In fact, liver damage must not be linked to the type of alcoholic beverages, but mostly to the ethanol amount contained in the drink and to the frequency of the taking, with less danger for such diseases in case of intermittent intake;
The nutritional condition: the nutritional state plays an important role in protecting the liver against alcohol-induced damage, at least in the case of a moderate intake. It has been shown that, sometimes, the hepatic damage due to an insufficient intake of protein and calories comes before the alcohol-related one, which often occurs in lower class individuals. In fact, malnutrition and alcohol hepatotoxicity seem to act in synergy.
COMPLICATIONS
The main complications of such kind of pathologies are portal hypertension with its typical features, as gastrointestinal bleeding, due to the spontaneous rupture and hemorrhage from esophageal varices; ascites; encephalopathy, with confusion and forgetfulness up to coma, following high blood level of ammonia; reduced levels of platelets or decreased white blood cell count. In the worst cases, it is possible to develop hepatocellular carcinoma and liver failure.
THERAPY
The most important measure to take is the immediate and complete ceasing of alcohol intake: the patient improvement is surprisingly very rapid. During the period of detoxification, a calorie-rich diet is necessary, reducing fat normal intake, which can interfere with ethanol hepatic metabolism, as well as an addition of vitamins (vit C, K and B-complex) and dietary minerals (including calcium and iron). Drug treatment is intended to relieve symptoms: it involves corticosteroids for severe cases (especially in presence of encephalopathy); colchicine to inhibit the progression of fibrosis; propylthiouracil to modify the metabolism in cirrhotic patients. If the therapy proves ineffective and no other treatment is available in a condition of severe liver failure, the last possibility is liver transplant. This theme evokes a lot of ethical question, but nowadays one of the criteria to become eligible for transplant is to discontinue alcohol consumption for a minimum of 6 months.
Treatment of alcoholic liver disease.2007
Sources:
Sheila Sherlock, James Dooley "Disease of the liver and iliary system"
L. Abenavoli ,I. Luppino, R. Spagnuolo "L’epatopatia alcolica: dal danno alla terapia"
Sandeep Mukherjee et al. "Alcoholic Hepatitis"
David C Wolf et al. "Cirrhosis"