DESCRIPTION
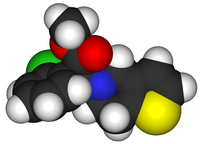
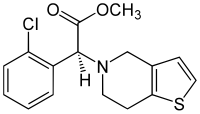
Clopidogrel is an antiplatelet agent structurally similar to ticlopidine. It is an oral, thienopyridine drug used in coronary artery disease, peripheral vascular disease and cerebrovascular disease. Its trade names are Plavix, Iscover, Clopilet, Ceruvin.
CLASSIFICATION
- Antiplatelet drug
- Fibrinolytic agent
INDICATIONS
Clopidogrel is indicated for:
-prevention of atherotrombotic events in patients at hight risk (multiple risk factors)
-treatment of acute coronary syndrome ( Non-ST segment elevation MI, ST segment elevation MI, unstable angina) in association with acetylsalicylic acid (aspirin)
-treatment of stroke
-treatment of peripheral vascular disease
-prevention of thrombosis after placement of intracoronary stent in association with ASA
-alternative antiplatelet drug for patients intolerant to ASA
PHARMACOKINETICS

Clopidogrel is an inactive pro-drug, meaning it has no direct pharmacological activity. The active metabolite, a thiol derivative, is formed in liver after two steps cytochrome P450 mediated ( mainly CYP2C19, CYP3A4). The first step is represented by the oxydation of clopidogrel to 2-oxo-clopidogrel, the subsequent step is a hydrolysis.
The active metabolite has an elimination half-life of about eight hours.
Absorption:
clopidogrel is rapidly absorbed with peak plasma levels (approx. 3 mg/L) of the main circulating metabolite occurring approximately one hour after dosing.
Distribution:
clopidogrel and the main circulating metabolite bind reversibly plasma proteins (98%).
Metabolism:
clopidogrel undergoes rapid hydrolysis into its carboxylic acid derivative. In plasma and urin you can also observe the glucuronide of the carboxylic acid derivative.
Elimination:
approximately 50% of clopidogrel is excreted in the urine and approximately 46% in the feces in the five days after dosing.
Food interaction:
administration of clopidogrel with other meals did not significantly modify the bioavailability of the drug.
Drug Interaction:
PPI: certain PPIs are known to inhibit liver enzymes, including CYP 2C19. This inhibition can decrease the activation of clopidogrel, lowering its efficacy and thus increasing the risk of cardiovascular events. Omeprazole is known to be one of the strongest inhibitors of CYP2C19.
Clinical studies are not concordant on clinical significance of this potential interaction, however the FDA warnings are:
- The concomitant use of clopidogrel with omeprazole should be avoided. Patients receiving these interacting medications may not receive the full anti-platelet effect of clopidogrel.
-Separating the administration times of clopidogrel and omeprazole does not reduce this drug interaction.
-The current warnings pertain only to omeprazole and esomeprazole (the S-enantiomer of omeprazole) . At this time, there is insufficient data to conclude that other proton pump inhibitors interact with clopidogrel.
Pharmacodynamic Impacts of Proton Pump Inhibitors on the Efficacy of Clopidogrel In Vivo-A Systematic Review, 2013
Other CYP2C19 inhibitors: amiodarone, cimetidine, fluconazole, ketoconazole, paroxetine, fluoxetine, valproic acid, isoniazid, ticlopidine. These drugs can decrease the activation of clopidogrel, lowering its efficacy and thus increasing the risk of cardiovascular events.
CYP2C19 inducers: dexamethasone, rifampin. These drugs increase the efficacy of clopidogrel, increasing the emorrhagic risk.
Statins: some statins (atorvastatin, simvastatin not pravastatin e rosuvastatin) may inhibit the antiplatelet effects of clopidogrel via competitive metabolism of its activating enzyme cytochrome P450 3A4 (CYP3A4). Different studies demonstrate the absence of clinical significance of this interaction.
Lack of evidence of a clopidogrel-statin interaction in the CHARISMA trial, 2007
Other CYP3A4 inhibitors: amiodarone,cimetidine, fluconazole, ketoconazole, paroxetine, fluoxetine, valproic acid, isoniazid, ciclosporine, grapefruit juice. These drugs can decrease the activation of clopidogrel, lowering its efficacy and thus increasing the risk of cardiovascular events.
CYP3A4 inducers: dexamethasone, rifampin, fenitoine, carbamazepine, fenobarbital. These drugs increase the efficacy of clopidogrel, increasing the emorrhagic risk.
Warfarin, Heparin: increased bleed risk may occur as a result of additive anticoagulant effects. Increase monitoring for signs and symptoms of bleeding during concomitant therapy.
MOLECULAR MECHANISM
The drug works by irreversibly inhibiting a receptor called P2Y12, an adenosine diphosphate (ADP) chemoreceptor on platelet cell membranes. The result is the inhibition of platelet.

PHARMACOGENOMICS
CYP2C19 is involved in the activation of the pro-drug clopidogrel.
Genetic polymorphism (mainly CYP2C19*2, CYP2C19*3 and CYP2C19*17) exists for CYP2C19, with approximately 3% of Caucasian and 15–20% of Asian populations.

These patients can be carriers of two or one loss of function, however they are called poor metabolisers and have dicreased CYP2C19 function.
Poor metabolisers have a reduction of 30-50% in the peak plasma and they are 1.5 to 3.5 times more likely to die or have complications (myocardial infarction, stroke) than patients with the high-functioning allele.
Genetic tests are available but are very expensive. They are indicated only for individuals with a personal or family history of adverse drug reactions to medications metabolized by CYP2C19.
For these idividuals is necessary to increase clopidogrel dose or change antiplatelet drug (Prasugrel and Ticagrelor are not metabolized by CYP2C19).
SIDE EFFECTS
Adverse drug reactions associated with clopidogrel are:
- neutropenia (incidence: 1/2.000)
- thrombotic thrombocytopenic purpura (incidence: 4/1.000.000)
- thrombocytopenia (0.2% severe cases as compared to 0.1% under aspirin)
- hemorrhage: digestive tract hemorrhage, cerebral hemorrhage, bleeding in the post operative period. The incidence of hemorrhage may be increased by the co-administration of aspirin. Use of non-steroidal anti-inflammatory drugs is discouraged in those taking clopidogrel due to increased risk of digestive tract hemorrhage.
- diarrhea,nausea
- rash
- respiratory (infrequent): upper respiratory infections, rhinitis, shortness of breath, cough
- cardiovascular: chest pain, edema
- gastric or duodenal ulcer, gastritis
- headache

TOXICITY
Symptoms of acute toxicity include vomiting (in baboons), prostration, difficult breathing, and gastrointestinal hemorrhage.
RESISTANCE
Research is being conducted to determine what influences an individual's response to clopidogrel; numerous mechanisms have been postulated. Noncompliance is a common cause for clopidogrel resistance. Variations in pharmacokinetics and pharmacodynamics may influence an individual's response to clopidogrel. Clopidogrel absorption varies between individuals, and there is significant interindividual variability in hepatic cytochrome P450 (CYP) 3A4 activity, thus drug-drug interactions could occur with other molecules metabolized by CYP3A4.
Resistance to clopidogrel: a review of the evidence, 2005
DOSAGE FORMS
Clopidogrel is marketed as clopidogrel bisulfate (clopidogrel hydrogen sulfate), as 75 mg and 300 mg oral tablets
Prevention: 75 mg/die.
NSTEMI,STEMI, unstable angina: 300 mg7die, then 75 mg/die.
Stent implantation: 300 or 600 mg before the procedure, then 75 mg/die.

Current evidence and future perspectives of omega-3 polyunsaturated fatty acids for the prevention of cardiovascular disease, 2013.
Polyunsaturated omega-3 fatty acids improve responsiveness to clopidogrel after percutaneous coronary intervention in patients with cytochrome P450 2C19 loss-of-function polymorphism, 2012..
Comparison of bleeding complications with omega-3 fatty acids + aspirin + clopidogrel--versus--aspirin + clopidogrel in patients with cardiovascular disease, 2009..
Results of the CAPRIE trial: efficacy and safety of clopidogrel. Clopidogrel versus aspirin in patients at risk of ischaemic events, 1998..
Aspirin in primary prevention
Aspirin for primary prevention of coronary heart disease: safety and absolute benefit related to coronary risk derived from meta-analysis of randomised trials, 2001.
Aspirin in secondary prevention
Update on aspirin in the treatment and prevention of cardiovascular disease, 2002.
Aspirin plus clopidogrel vs aspirin, in primary and secondary prevention
The CHARISMA study: in search of the best antiplatelet strategy for cardiovascular prevention, 2006.
Efficacy of omega 3 in secondary prevention
Beyond lipids: the role of omega-3 fatty acids from fish oil in the prevention of coronary heart disease, 2007.