Retinoids (vitamin A and its natural and synthetic congeners) are fat-soluble signaling molecules that are mainly derived from the diet as preformed vitamin A (or retinyl esters), which is found in animal foods (liver, milk, kidney, fish oil), fortified foods, and drug supplements. Dietary vitamin A is also obtained from provitamin A carotenoids from plant sources, principally carrots.
Vitamin A can be found in two principal forms in foods:
•Retinol, the form of vitamin A absorbed when eating animal food sources, is a yellow, fat-soluble substance.
After absorption, retinol is transported via chylomicrons to the liver.
•Carotenoids (alpha-carotene, beta-carotene and gamma-carotene); The enzyme 15-15'-dioxygenase converts carotenoids to retinal.
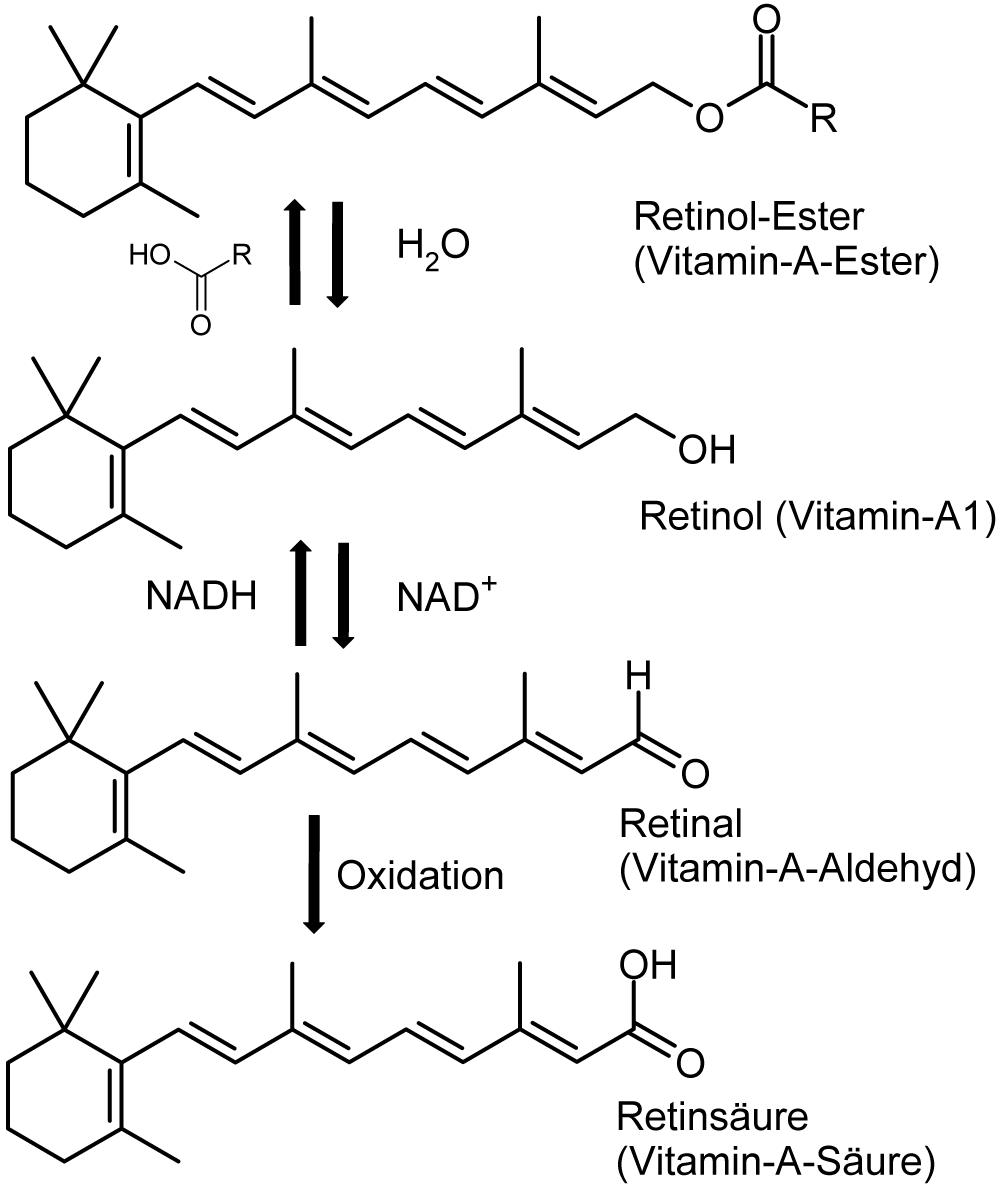
In the organism vitamin A is available in three forms:
• Retinol (ROL) The retinol form functions as a storage form of the vitamin.
• Retinaldehyde, or retinal. Converted from retinol by retinol dehydrogenase.
• Retinoic Acid (RA). Converted from retinal by retinaldehyde deidrogenase. This oxidation is an irreversible step.
In circulation it is bound to retinol-binding protein (RBP).
About 80% of the body stores of vitamin A are contained in the liver, in quantities sufficient to last the average adult about two years without the need for additional intake.
Serum ROL levels remain stable due to a carefully regulated transport system that ensures the target tissues receive the necessary amounts of ROL despite major fluctuations in dietary intake.
Functions
Vitamin A plays a role in a variety of functions throughout the body, such as:
• Vision: specifically related to the retinal form. Within the eye, 11-cis-retinal is bound to protein "opsin" to form rhodopsin in rods and iodopsin (cones). It's important for the mechanism of transduction.
• Gene transcription: Retinoic acid exerts its effects by binding to and activating two types of nuclear protein receptors: the RARs and RXRs (rexinoids, RXRs), both of which exist as three distinct gene products (alpha, beta, and gamma). These receptors control the expression of numerous target genes by binding to specific DNA sequences termed RA response elements (RAREs).
• Immune function: vitamin A stimulates functioning of the immune system in the body and increases its resistance to infections.
• Embryonic development and reproduction: It accelerates the synthesis of collagen and elastin fibres by fibroblasts, as well as the processes of cell division, thanks to which it stimulates growth of fetus and young organisms.
• Bone metabolism: Vitamin A positively influences the development of skeleton by regulating activities of osteoblasts and osteoclasts.
•It participates in hormonal regulation of the body by decreasing secretion of thyroxin (one of thyroid hormones) by means of suppressing production of thyrotropin by the pituitary gland.
• Hematopoiesis
• Skin healt: It ensures proper proliferation and differentiation of epithelial cells, contributing also to their regeneration
• Cellular health
• Antioxidant activity: A vital property of vitamin A is also its antioxidative action, including both prevention against reactive oxygen species (ROS) and termination of reactions taking place with their participation.
Vitamin A metabolism: an update. Nutrients. 2011
From carrot to clinic:an overview of the retinoic acid signaling pathway. 2010
Wikipedia
Types of Toxicity
While retinoids in low concentrations act in this way, higher concentrations are pro-oxidant, cytotoxic, mutagenic, and teratogenic, especially when unbound to protein.
Vitamin A toxicity is due mainly to excessive dietary intake or to self-medication, when the liver becomes saturated with vitamin A and stored retinyl esters spill over into the circulating blood. Retinyl esters react more randomly with cell membranes than the physiologically-sequestered RBP and hence are a major form of vitamin A toxicity.
Acute Toxicity- such as over a period of hours or a few days. Less of a problem than chronic toxicity.
In general, acute toxicity occurs at doses of 150–1200 mg (in International Units: 500 000–
–4 000 000 IU).
Children can reach toxic levels at 22- 45 mg (75 000 - 150 000 IU).
An extreme case was a fatal poisoning of polar explorers after the consumption of polar bear liver
(where vitamin A content is approx. 10 mg/g).
Chronic Toxicity - The chronic poisoning results from the long-term intake of this vitamin (ranging from several weeks to more than 3 years) at the doses > 30 mg (100 000 IU)/d by adults, or for 2 to 6 months at the doses of 3–9 mg (10 000–30 000 IU)/d by children, and for 1–3 months at
the dose of 3 mg (10 000 IU)/d by infants.
Effect of hypervitaminosis A
Retinoid toxicity is associated with high-to-normal or even low circulating retinol concentrations, and with increased fractions of retinyl esters circulating with plasma lipoproteins and not bound to retinol-binding protein (RBP).
poisoning referred to as hypervitaminosis A comes at blood concentration of the vitamin a > 1.0 mg/l (3.5 μmol/l).
The symptoms of acute poisoning are: general weakness, dizziness and a severe headache (in the occipital part), an increase in intracranial pressure, nausea, vomiting, sitophobia, hepatosplenomegalia, and after a few days, skin changes (itching, erythema, and desquamation).
The chronic poisoning symptoms include: feeling of chronic fatigue, irritability, double vision, nystagmus, sleep disturbances, cracking and bleeding lips and gums, shedding of hair, rashes and ulceration of the skin, muscular coordination disturbances, renal dysfunction (haematuria), and even oedema of the optic disc and other symptoms that could suggest a brain tumor.
The excessive intake of vitamin A affects harmfully the haematopoietic system, leading to aplastic anemia. It accelerates erythrocyte sedimentation rate and prolongs the prothrombin time. It also causes leukopaenia, weakening at the same time the defense ability of the body.
Another consequence of the excessive supply of vitamin A is the disruption of absorption of β-carotene and mineral salts from food.
Taking excessive amounts of vitamin A is also harmful for the osteoarticular system. It leads to joint and spine pains, as well as decalcification of bones (with the increase of calcium concentration in blood), which causes their brittleness and increases the risk of osteoporosis, and – as a result – also femoral neck fractures. Some researchers have posited also that another result of vitamin A overdose is the decrease of bone mineral density (BMD).
The above-mentioned effects are exacerbated by alcohol consumption.
High doses of vitamin A must not be administered in liver failure and cirrhosis or in bile ducts obstruction, due to the increase in the risk of toxic effects described above.
These high doses should be avoided during pregnancy, due to their contribution to fetal development anomalies (teratogenic activity).
Patients with hepatic and renal diseases and children are especially susceptible to the adverse effects
of this vitamin.
Vitamin Toxicity
Adverse effects of antioxidative vitamins: http://link.springer.com/article/10.2478%2FS13382-012-0022-x
Wikipedia
Altered fat-soluble vitamin metabolism
Vitamin A is fat-soluble and high levels have been reported affect metabolism of the other fat-soluble vitamins D, E and K.
The toxic effects of Vitamin A might be related to altered Vitamin D metabolism, concurrent ingestion of substantial amounts of Vitamin D or binding of Vitamin A to receptor heterodimers. There have been reported antagonistic and synergistic interactions between these 2 vitamins as they relate to skeletal health.
It has been reported that stimulation of bone resorption by Vitamin A is independent of it's effects on Vitamin D.
Is vitamin A consumption a risk factor for osteoporotic fracture?
Diagnosis
Tests may include:
•bone x-rays
•blood calcium test
•cholesterol test
•liver function test
•blood test for Vitamin A (Retinol esters as markers).
Prevention
Hypervitaminosis A can be prevented by not ingesting more than the Tolerable Upper Level of intake for Vitamin A. This level is for synthetic and natural retinol ester forms of vitamin A. Carotene forms from dietarysources are nottoxic. The dose over and above the RDA is among the narrowest of the vitamins and minerals. Possible pregnancy, liver disease, high alcohol consumption, and smoking are indications for close monitoring and limitation of vitamin A administration.
Vitamin E - may alleviate hypervitaminosis A.
Retinoic Acid Syndrome
Retinoic acid syndrome is a novel complication of therapy with all-trans retinoic acid (ATRA) in patients with acute promyelocytic leukemia (APML). Primarily the syndrome consists of fever and respiratory distress. Additional features include weight gain, oedema over lower extremities, pleural or pericardial effusion and hypotension.
Retinoic acid syndrome
Synthetic retinoids
For the treatment of acne, the most prescribed retinoid drug is 13-cis retinoic acid (isotretinoin). It reduces the size and secretion of the sebaceous glands. Although it is known that 40 mg of isotretinoin will break down to an equivalent of 10 mg of ATRA — the mechanism of action of the drug (original brand name Accutane) remains unknown and is a matter of some controversy. Isotretinoin reduces bacterial numbers in both the ducts and skin surface. This is thought to be a result of the reduction in sebum, a nutrient source for the bacteria. Isotretinoin reduces inflammation via inhibition of chemotactic responses of monocytes and neutrophils.
Isotretinoin also has been shown to initiate remodeling of the sebaceous glands; triggering changes in gene expression that selectively induce apoptosis.
Isotretinoin is a teratogen with a number of potential side-effects. Consequently, its use requires medical supervision.


Synthetic retinoids irritate skin and mucosa, causing erythema, rash, contact dermatitis and loss of hair, and exacerbate the symptoms in patients with psoriasis. They impair liver functions, what may be manifested in blood by increased activities of various enzymes, e.g. ALAT (ala nine aminotransferase), AspAT (aspartate aminotransferase) and LDH (lactate dehydrogenase), increased lipid profile with the decrease of the level of HDL (high-density lipoprotein), as well as increased concentrations of metabolites such as bilirubin and uric acid. The resultant toxic effects disrupt also composition and properties of the blood itself, leading to anaemia, neutropenia, acceleration of erythrocyte sedimentation rate (ESR) and coagulability disorders. Like vitamin A, synthetic retinoids increase the risk of osteoporosis. Also, they show embryotoxic and teratogenic activity, so they must not be used during pregnancy and lactation, even at low doses.
Potential risk of high intake of β-carotene
For a long time β-carotene, considered only as provitamin A, was believed to be practically harmless. It was stressed that its enzymatic conversion to retinol (in liver and small
intestine wall), thanks to homeostatic control, provided only as much vitamin A as required by the body due to a temporary deficiency, and that β-carotene excess was expelled in faeces. This opinion was confirmed by an observation that even a long-standing supplementation with β-carotene (25 mg/d) did not cause hypervitaminosis A with its effects as described above, provided that no preparations of vitamin A were taken at the same time.
Research has shown that β-carotene is not embryotoxic.
Prolonged intake in large doses is a yellowish skin tinge, known as carotenemia .

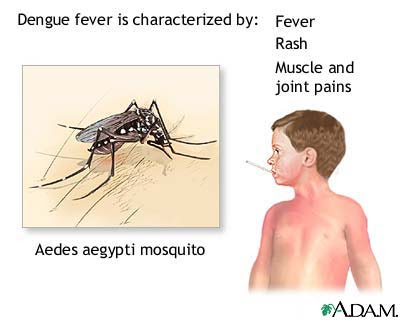
Role in Dengue Hemorrhagic Fever
interactions between dengue viruses and retinoids in the liver, triggering viral replication
and disease pathogenesis, and that disease manifestations (e.g., fever, severe arthralgia, bone pain, plasma leakage, thrombocytopenia, headache, and gastrointestinal symptoms) are caused by the damaging effects of dengue virus-induced activation of hepatocytes and the resulting spillage of toxic retinoids (i.e., retinyl esters and retinoic acid) into the circulation.
There are strong parallels between the manifestations of DHF and those of hypervitaminosis
A. Most if not all of the signs and symptoms of DHF have a counterpart in the manifestations of hypervitaminosis A (see Table 1, below).
The hypothesis proposed is that the diverse manifestations of DHF are due to interactions between dengue virus and endogenous retinoids (vitamin A and its congeners), leading to retinoid
receptor-induced activation of hepatic stellate cells and damage to the liver and the spillage of stored retinoids into the circulation in toxic concentrations.
Dengue virus infection activates the retinoid cascade in the liver, leading to increased retinoic acid production and retinoic acid receptor (RAR) activation and expression within the hepatic
cell nuclei, causing inflammation and liver damage.
Retinoic acid and stored retinyl esters released into the circulation from damaged liver cells cause the manifestations of DHF via apoptosis and necrosis.
Kupffer cells, in addition to being the source of macrophages in the liver, play a critical role in hypervitaminosis A. Vitamin A activates Kupffer cells through INF-c production by activated
T-lymphocytes, and activated Kupffer cells potentiate liver toxicity even with low levels of other hepatotoxins such as alcohol.
Retinoids, race and the pathogenesis of dengue hemorrhagic fever(13)00393-9/abstract
Role in Malaria
The characteristic hemolysis and anemia of malaria and other symptoms of the disease may thus be manifestations of an endogenous form of vitamin A intoxication associated with high concentrations of RA but low concentrations of retinol (ROL). Retinoic acid released from the parasites may also affect the fetus and cause preterm birth and fetal growth restriction (FGR) as a function of the membranolytic and growth inhibitory effects of these compounds, respectively. Subject to testing, the hypothesis suggests that parasite vitamin A metabolism could become a new target for the treatment and prevention of malaria.
On this hypothesis, the parasites emerge from the liver packed with vitamin A and use
RA as a cell membrane destabilizer to invade the red blood cells (RBCs), causing hemolysis and anemia.
Other symptoms of the disease – e.g., fever, headache, muscle aches, gastrointestinal symptoms, seizures, coma, respiratory distress, and retinopathy – may similarly reflect parasite-induced vitamin A toxicity in the brain and other organs, following the transport of RBCs throughout the body and the release of RA (or RAs) into the circulation. It is further suggested that RA released from the parasites also enters the fetus and causes preterm birth and/or intrauterine growth restriction and low birth weight as a function of the membrane destabilizing and growth inhibitory effects of retinoids. This prediction, that low serum ROL concentrations in malaria.
The pathogenesis of malaria: a new perspective