Introduction
This rare disease was first described by German neurologist Hans Creutzfeldt and Alfons Jakob in 1920, giving it the name Creutzfeldt–Jakob disease (CJD). CJD is a family of human and animal diseases known as the transmissible spongiform encephalopathies caused by prion proteins. The term spongiform refers to the characteristic appearance of infected brains, which become filled with holes until they resemble sponges under a microscope. It affects about one person in every one million people per year worldwide; in the USA there are about 300 cases per year. CJD usually appears in later life and runs a rapid course. Typically, onset of symptoms occurs about age 60, and about 90 percent of individuals die within 1 year. In the early stages of disease, people may have failing memory, behavioral changes, lack of coordination and visual disturbances. As the illness progresses, mental deterioration becomes pronounced and involuntary movements, blindness, weakness of extremities, coma and death

Spongiform degeneration of the brain in CJD
Clinical and instrumental diagnosis of CJD
The diagnosis of Creutzfeldt–Jakob disease is based on : 1)clinical syndrome and 2) instrumentals tests (EEG, CSF analysis and cranial MRI) . The predominant clinical symptoms are characterized by rapid progressive dementia followed by development of neurological signs, e.g. ataxia and myoclonus. The disease is fatal and leads to death in a few months. Various instrumentals diagnostics methods are commonly used. Detection of periodic sharp wave complexes on EEG substantiated the diagnosis of sporadic CJD disease for a long period of time . Another major step in the diagnosis of sporadic CJD was the introduction of MRI, where a specific pattern of alterations characterized by hyperintense signals in basal ganglia and cortical regions, was identified. As a result, a positive MRI scan was proposed to be included into the clinical criteria in 2009.
The Role of Neuroimaging in Evaluating Patients Affected by Creutzfeldt-Jakob Disease: A Systematic Review of the Literature, 2014
From 1996 onwards, detection of neuronal destruction markers in CSF have become more and more important. They have been established in diagnostic work-up, with protein 14-3-3 as the most promising surrogate marker finally included in the WHO criteria in 1998 and in guideline of American Academy of Neurology in 2012. Because elevated levels of protein 14-3-3 are also reported in a range of non-prion-related diseases, mostly caused by an acute neurological event such:encephalitis, stroke, or tumour, positivity of the results must be interpreted in the clinical and instrumental context.

MRI in CJD: hyperintense signals in basal ganglia and thalamus (arrows)
Protein 14.3.3
The 14-3-3 proteins are a family of conserved regulatory molecules that are expressed in all eukaryotic cells. The family consist of 7 isoform named: beta,gamma,epsilon,eta,sigma,theta and zeta. All are phosphoserine/threonine binding proteins.
How do 14-3-3 proteins work?-- Gatekeeper phosphorylation and the molecular anvil hypothesis., 2002
The 14-3-3 proteins can be considered evolved members of the Tetratrico Peptide Repeat (TPR) superfamily, generally have 9 or 10 alpha helices, and usually form homo- and/or hetero-dimer interactions along their amino-termini helices.
The 14-3-3 proteins have the ability to bind a multitude of functionally diverse signaling proteins, including kinases, phosphatases, and transmembrane receptors and are involved in many vital celllular processes such metabolism, protein trafficking, signal transduction, apoptosis and cell cycle regulation. The molecular weight is about 30 Kd.
The 14.3.3 is present in many human tissues: kidney, liver,lung, bone, pancreas, nervous system ecc.; more than 200 signaling proteins have been reported as 14-3-3 ligands.
The name 14-3-3 refers to the particular elution and migration pattern of these proteins on DEAE-cellulose chromatography and starch-gel electrophoresis. Elevated amounts of 14-3-3 proteins are found in the cerebrospinal fluid of patients with CJD.
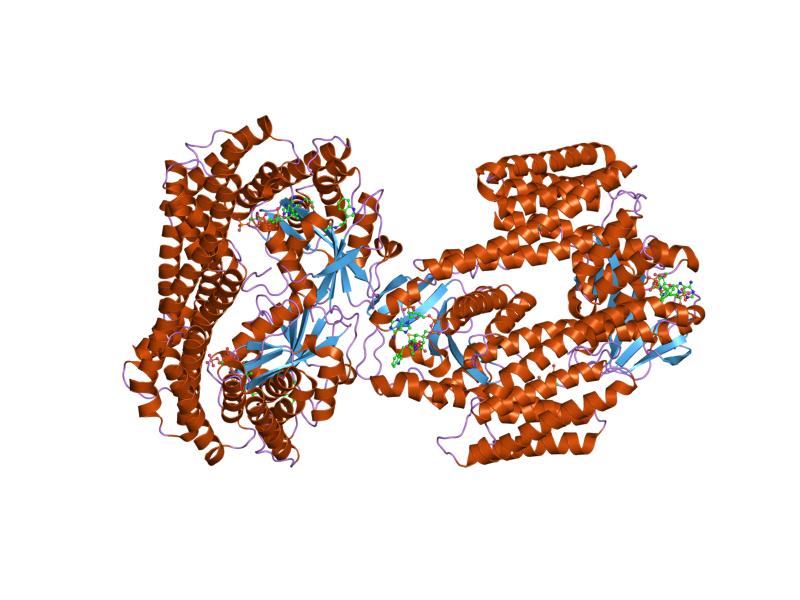
Molecular structure of a 14-3-3 protein dimer
14-3-3 protein
Specificity of Protein 14-3-3
A positive CSF 14-3-3 test displays one of the important diagnostic tools in the identification of patients with CJD disease at present because from technical point of view this marker is stable and CSF samples can be forwarded for testing to specialized laboratories. Meanwhile, the test is widely available and serves as an important tool in surveillance studies worldwide.. A large number of studies proved that in the appropriate clinical circumstances a positive 14-3-3 test is highly sensitive and specific for sporadic CJD diagnosis.
Evidence-based guideline: diagnostic accuracy of CSF 14-3-3 protein in sporadic Creutzfeldt-Jakob disease: report of the guideline development subcommittee of the American Academy of Neurology. , 2012
Protein 14-3-3 detection correlated with clinical diagnosis in 85–94% in sporadic CJD. Specificities ranging from 84% and 85% to 100% in the literature. The majority of studies on national and multicentre levels reported a 14-3-3 specificity >90% However there is a number of positive tests related to non-CJD disease diagnosis mostly of acute neurological origin.
Rapid dementia caused by acute neurological events (e.g. inflammation, stroke, CNS tumour or epileptic fits) is the main reason for a drop in test specificity from 92% to 82–85%. If tested in the context of neurodegenerative disease alone, the test specificity was high (95–97%). A careful interpretation of a positive 14-3-3 test in the clinical context is therefore mandatory to exclude acute neurological events which is easily achieved taken together information on basic CSF results as well as imaging results (MRI for exclusion of tumour, encephalitis and stroke) and EEG (epileptic pattern) together with the thorough ascertainment of the patient's clinical history.

Conclusion
The literature data demonstrates that CSF protein 14-3-3 detection remains an important test in the diagnosis of CJD. Due to a loss in specificity in acute neurological events, the interpretation of positive 14-3-3 results needs to be performed in the clinical context. The spectrum of differential diagnosis of rapid progressive dementia included those of neurodegenerative origin, dementia in acute neurological diseases as well as from non-neurological origin.