Giulia Gallo
Veronica Mulatero
DESCRIPTION
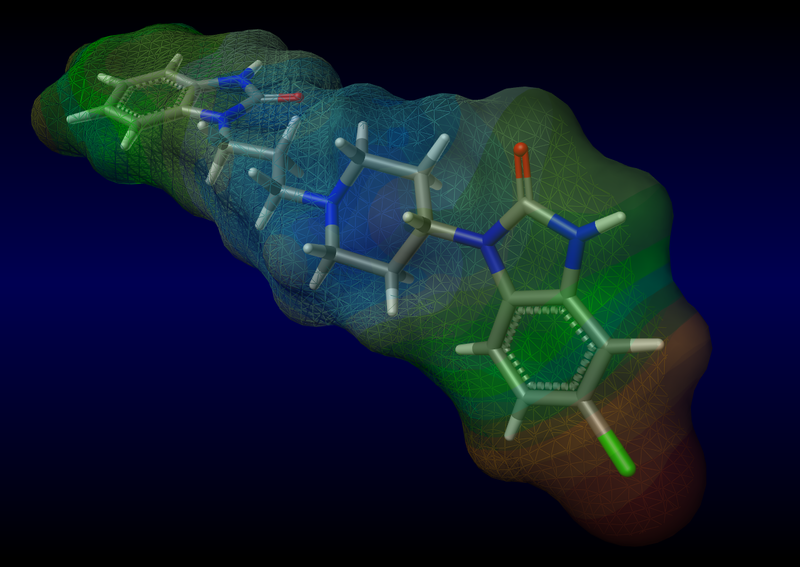

Empirical formula: C22H24ClN5O2; Molecular mass: 425.911 g/mol; Code ATC: A03FA03
Domperidone is a dopamine antagonist (it acts by antagonizing the D2 receptor) with anti-emetic properties. It does not cross the bloodbrain barrier. Its anti-emetic effect may be due to a combination of peripheral (gastrokinetic) effects and antagonism of dopamine receptors in the chemoreceptor trigger zone, which lies outside the blood-brain barrier in the area postrema. Studies in man have shown oral domperidone to increase lower oesophageal pressure, improve antroduodenal motility and accelerate gastric emptying. There is no effect on gastric secretion.

CLASSIFICATION
D2 antagonist receptor.
THERAPEUTIC INDICATIONS
Domperidone is used for the relief of nausea and vomiting, epigastric sense of fullness, upper abdominal discomfort and regurgitation of gastric contents.It’s useful especially when these last less than 48hours. It is also used to treat nausea and vomiting caused by some drugs ( levodopa) used to treat Parkinson's Disease and by brain disease like concussion, migraine and tumor.
FARMACOKINETIC PROPERTIES
Absorption: the drug is rapidly absorbed after oral administration with peak plasma concentrations at 30 to 60 minutes. The low absolute bioavailability of oral domperidone (15%) is due to an extensive first-pass metabolism in the gut wall and liver. Patients with gastrointestinal complaints should take domperidone 15-30 minutes before a meal. Reduced gastric acidity impairs the absorption of domperidone. Oral bioavailability is decreased by cimetidine and sodium bicarbonate.
Distribution: oral domperidone does not appear to accumulate or induce its own metabolism; a peak plasma level after 90 minutes (21ng/ml) after two weeks oral administration of 30 mg per day was almost the same as that of 18 ng/ml after the first dose. Domperidone is 91-93% bound to plasma proteins. It seems to have a good tissue distribution, but low brain concentration. Small amounts of drug cross the placenta in rats. The plasma half life after a single oral dose is 7-9 hours in healthy subjects but is prolonged in patients with severe renal insufficiency.
Metabolism: domperidone undergoes rapid and extensive hepatic metabolism by hydroxylation (CYP3A4, CYP1A2 and CYP2E1) and N-dealkylation (CYP3A4).
Excretion: urinary and faecal excretions amount to 31 and 66% of the oral dose respectively.
MOLECULAR MECHANISM
Domperidone antagonizes the D2 receptor. D2 belongs to a large superfamily of GPCRs. Dopamine receptors show a high degree of similarity in their primary amino acid sequences, have a common structure of seven transmembrane-spanning domains and are capable of activating heterotrimeric G proteins to induce intracellular signaling mechanism.

Dopamine receptor structure. Structural features of D1-like receptors are represented. D2-like receptors are characterized by a shorter COOH-terminal tail and by a bigger 3rd intracellular loop.
Early and late D2 dopamine receptor signaling during slow synaptic transmission: in the early phase of signaling, G protein-mediated signaling induces a rapid and transient change in the phosphorylation of PKA targets such as DARPP-32 and CREB. This early phase of D2 dopamine receptor signaling is rapidly antagonized after the inactivation of G proteins by RGSs. In addition, receptor phosphorylation by GRKs results in G protein uncoupling, recruitment of β-arrestins, and clathrin-dependent receptor internalization, effectively shutting down G protein-mediated signaling. In the late phase of signaling, the D2 dopamine receptors stimulate the formation of a protein complex composed of β-arrestin 2, PP2A, and Akt. Formation of this complex results in the deactivation of Akt by PP2A and the subsequent stimulation of GSK-3-mediated signaling. This second wave of signaling mediated by the Akt/β-arrestin 2PP2A complex results in a more progressive and longer lasting response. AP2, adaptor protein complex; DA, dopamine; D2R, D2 dopamine receptor.

The Physiology, Signaling, and Pharmacology of Dopamine Receptors, 2014
POSOLOGY
It is recommended to take domperidone tablets (10 mg dose) before meals. If taken after meals, absorption of the drug is delayed.

For the relief of symptoms of post-prandial stomach discomfort,in adults and children 16 years of age and older: up to 10 mg three times daily and at night. Maximum duration of course of treatment 2 weeks.
For the relief of nausea and vomiting, adults and children 16 years of age and older: up to 10 mg three times daily and at night. Maximum duration of course of treatment 48 hours.
Use in children under 16 years of age: not recommended.
posology
SIDE EFFECTS
-sonnolence, headache(un common)
-breast pain, breast tenderness(uncommon)
-asthenia(uncommon)
-loss of libido,anxiety (uncommon)
-diarrhoea( uncommon), dry mouth (common)
-possible side effects (not proved with studies, post marketing experience useful): anaphylactic reactions including anaphylactic shock, angioedema, allergic reaction, agitation, nervousness or somnolence, convulsions, oculogyric crisis, urticaria, angioedema, liver function test abnormal.
-as the pituitary is outside the blood brain barrier, domperidone may cause an increase in prolactin levels. In rare cases this hyperprolactinaemia may lead to neuro-endocrinological side effects such as galactorrhoea, gynaecomastia and amenorrhoea.
-extrapyramidal side effects are very rare in neonates and infants, and exceptional in adults. These side effects reverse spontaneously and completely as soon as the treatment is stopped.
pharmacology of domperidone
FOCUS ON CARDIOVASCULAR EFFECT OF DOMPERIDONE
information note on Domperidone (14/11/2011),AIFA
Many scientific studies evidenced that domperidone could be associated with risk of sudden cardiac death or ventricular arrhythmia. This could be higher in patients older than 60 or for oral administration higher than 30 mg. Thus the drug should be used at minimum dosage in adults and kids. The cardiac risk is monitored in Italy and in other states from many years.
Motilium: the risk of prolonging of the QTc and cardiac problems is explicated on the leaflet since febrarby 2004. It was updated in 2008, and in 2010 two epidemiological studies were published. Evidences suggest that high dosage (>30mg/die) or patients older than 60 can be at risk of sudden cardiac death and arrhythmias.
Thus health workers have to be aware of this risks and have to be careful to use domperidone in patients with long QTc, with electrolyte disturbances and previous cardiac insufficiency.
AIFA NOTE ON DOMPERIDONE
“Risk of serious ventricular arrhythmia and sudden cardiac death in a cohort of users of domperidone: a nested case-control study”:
Catherine B. Johannes,Cristina Varas-Lorenzo,Lisa J. McQuay, Kirk D. Midkiff and Daniel Fife.Article first published online: 22 JUL 2010.DOI: 10.1002/pds.2016”
In 2010 a nested case-control study tried to describe this relationship, comparing the use of oral domperidone or PPI in a larger population with noted clinical informations. Patients were83 212 in the exposure cohort, enrolled in the Saskatchewan Health (a provincial government ministry) and were studied for one year after the therapy’s beginning.
All cases of ventricular arrhythmia (ventricular tachycardia, ventricular fibrillation, flutter and cardiac arrest due to this causes, sudden cardiac death) were studied by cardiologists, who didn’t know the therapy of each patient.
Many of the potential confounders evaluated were strong individual predictors of SVA/SCD, in particular a history of VT/VF, current exposure to QT prolonging medications, and the presence in the year before of heart disease, liver failure, exposure to cardiac medication. Compared with non-users of domperidone or PPI, the OR for SVA/SCD among current domperidone users was 1.67 (95%CI) and among current users of both domperidone and PPI was 2.09 (95%CI). In the multivariate adjusted analysis, the increased risk of SVA/SCD was attenuated in current domperidone users (OR: 1.59, 95%CI) and in current users of both (OR: 1.39, 95%CI). Past domperidone exposure was not associated with increased risk of SVA/SCD. A 53% increased risk with current PPI use was noted in analyses adjusted for variables, but multivariate adjustment established a risk of 11%. The adjusted OR for current domperidone versus current PPI use was 1.44. In stratified analyses the adjusted OR for current domperidone exposure compared with non-use was higher in case-control pairs without diabetes, in those older than 60 years, and in males, but there are few cases analyzed.
Current domperidone use was associated with a 44% increase in the risk of SVA/SCD compared with current PPI exposure, and a 59% increase compared with non-use. The domperidone versus PPI comparison found that the domperidone outcome effect estimate was still elevated but lower than the domperidone versus non-use comparison. The unadjusted OR for current domperidone use was 5.4 and the OR adjusted for diabetes, arrhythmias, heart failure, hypertension, cerebrovascular and cardiovascular ischemia, smoking, alcohol abuse, and current use of cardiac glycosides and diuretics was 3.8.
CONCLUSION: Consistent with this result and with the higher effect documented in first-time users of different types of medications in several outcomes, we found that the OR of SVA/SCD was highest in current domperidone users with only one dispensing and decreased with an increasing number of consecutive dispensings in subjects 60 years and older. Administrative databases have limitations including lack of information about disease severity and important risk factors, lack of physiologic or electrocardiogram data in which to assess QT prolongation, and limited ability to assess data validity. The study lacked information on smoking and some specific triggers (digitalis toxicity, hypokalemia, hyperkalemia, or hypomagnesemia).
Also, we lacked information on prescribed dose, actual use, and medical compliance. Therefore, we could not determine whether there was a dose-response relationship between domperidone and SVA/SCD. Furthermore, nonprescription medication usage is not captured.
article
Domperidone and Ventricular Arrhytmia or Sudden Cardiac Death: a population-based case-control study in the Netherlands
van Noord C, Dieleman JP, van Herpen G, Verhamme K, Sturkenboom MC. 1 nov2010, Drug Saf.
Another study used the Integrated Primary Care Information database of Netherlands.
Background: the prolongation of QT due to the action of domperidone seems to be related with the inhibition of the hERG K+delayed rectifier channel in heart. This action cause a significant prolongation of cardiac repolarization. This channel has a structure like following A image:

The study included patients aged >18 years without cancer, considering the same co-variates and bias of the other previously reported; it was based on a case-control method. Authors considered also at the end the exclusion of diabetes mellitus and cardiovascular disease. Controls were randomly drown (using a double-blind method) from the source population and matched to cases on age, sex, practice and index rate. The study population comprised 1366cases and 14114matched controls, valued during one year of database capture. All subjects were followed until the outcome of interest (SCD, non fatal VA, both), cancer, death, transferring out of the practice. All analyses were furthermore stratified by insurance. The association between the use of domperidone by recency of use (current, past, never use) and daily dose(<30, 30, >30 mg/die) and the risk of SCD and SVA were studied as outcomes. Of all cases 10patients were current users of domperidone and all had SCD. The matched unadjusted OR of domperidone use and SCD was 3.72. Daily doses >30mg were associated with a significant increased risk of SCD (adjusted OR=11.4). Current use was associated with significant increased risk of SCD (OR 4.17); in privately and non insured patients scientists could not estimate the adjusted effect of current use of domperidone because of small numbers of exposed. The matched OR unadjusted for current use was 0.78 for privately insured patients and 1.73 for non-insured. A high daily dose was associated with a higher risk of SCD after complete adjustment than normal-low dosage (OR 11.4 versus 1.02 and 1.24). As conclusion, the study says that current use of domperidone, especially high doses, is associated with an increase of SCD but can’t demonstrate an effect on non fatal VA due to absence of exposed cases.
article
TOXICITY
lactose intolerance, galactosaemia or glucose/galactose malabsorption: it can be unsuitable because containing lactose.
Use during lactation: the total amount excreted in human breast milk is expected to be less than 7 micrograms per day at the highest recommended dosing regimen. It is not known whether this is harmful to the newborn. Therefore breast-feeding is not recommended for mothers who are taking domperidone. It should also be avoided in pregnancy.
Use in infants: since metabolic functions and the blood-brain barrier are not fully developed in the first months of life the risk of neurological side effects is higher in young children. Therefore, it is recommended that the dose be determined accurately and followed strictly in neonates, infants, toddlers and small children.
Use in liver disorders: since domperidone is highly metabolised in the liver, domperidone should be not be used in patients with hepatic impairment.
Renal insufficiency: in patients with severe renal insufficiency (serum creatinine > 6 mg/100 mL) the elimination half-life of domperidone was increased from 7.4 to 20.8 hours, but plasma drug levels were lower. Since very little unchanged drug is excreted via the kidneys, the dose of a single administration don’t to be adjusted. However, on repeated administration, the dosing frequency should be reduced to once or twice daily depending on the severity of the impairment, and the dose may need to be reduced. Such patients on prolonged therapy should be reviewed regularly.
Use with CYP3A4 inhibitors: co-administration with oral ketoconazole, erythromycin or other potent CYP3A4 inhibitors that prolong the QTc interval should be avoided.
Cardiovascular effects: see focus ay the end.
DRUG INTERACTIONS
Using domperidone with any of the following medicines is not recommended. The therapy has to be changed with: Amifampridine, Cisapride, Dronedarone, Fluconazole, Ketoconazole, Mesoridazine, Pimozide, Piperaquine, Posaconazole, Sparfloxacin, Thioridazine, Ziprasidone.
The use of drugs like one of the following is not avoided but also not recommended; it should be communicated to the doctor: Amiodarone, Amitriptyline, Amlodipine, Apomorphine, Atorvastatin, Azithromycin, Boceprevir, Chloroquine, Chlorpromazine, Cimetidine, Ciprofloxacin, Citalopram, Clarithromycin, Clomipramine, Clozapine, Cyclosporine, Dasatinib, Diltiazem, Disopyramide, Erythromycin, Flecainide, Fluoxetine, Imatinib, Imipramine, Indinavir, Isoniazid, Itraconazole, Levofloxacin, Lithium, Methadone, Nefazodone, Nilotinib, Nortriptyline, Octreotide, Ondansetron, Procainamide, Promethazine, Propafenone, Quinidine, Quinine, Ranitidine, Ranolazine, Ritonavir, Salmeterol, Sodium Phosphate, Solifenacin, Sorafenib, Trazodone, Vardenafil, Verapamil, Vilanterol, Voriconazole.
PHARMACOGENOMICS
RESISTANCE
DEPENDENCE AND WITHDRAW