DEFINITION
Schizophrenia (see also here) is a debilitating chronic psychiatric syndrome that affects 1% of the adult population, characterized by a course of more than six months and the persistence of abnormal thinking, behavior, and emotions.
The term actually means a class of disorders that vary in severity and progression. The etiology is complex (genetic, morphological, environmental, social ...) and still unclear.
EPIDEMIOLOGY
Schizophrenia is a disorder that occurs most frequently in adults aged 15 to 25 years.
The prevalence in the general population is about 1%. The prevalence among first-degree relatives of people affected is: 5-12%; there is a concordance of 50-65% among monozygotic twins; while in dizygotic twins it is equal to 5-12%.
The disease tends to occur earlier in males than in females. In females the event is late: usually around 30-35 years. The late-onset forms are generally better prognosis because they present a predominance of positive symptoms (and therefore a better response to drug therapy) and a minor frequency of disorganization and negative symptoms. There is also a greater preservation of: basic personality, affect and social functioning.
SYMPTOMS
There are three clinical phases :
• Premorbid
• Prodromal
• Overt disease (active phase or state period)
The Premorbid Phase
The vulnerability of schizophrenia may be evident before the onset of a disease in the form of a premorbid and inadequate functioning: 50% of future schizophrenics do not have a particular premorbid personality; 25% non-specific traits (emotional sensitivity, difficulty in keeping with the others, etc.); the remaining 25%, represented mainly by children of parents with schizophrenia, presents premorbid personality characterized by introversion, isolation or withdrawal, distrust, poor social skills, mild cognitive impairment (attentional, poor arithmetic skills), weird and eccentric behavior, pseudo-depressive aspects with disregard for the usual activities carried out by coetaneous (sports, the opposite sex), poor ability to emotionally connect, irrelevant psychomotor abnormalities (neurological soft sign), interest-philosophical-religious-esoteric astrology.
The Prodromal Phase
In the next phase , there is a change from the status of previous operation, often after a normal event experienced as stressful by the subject (exams, university, military, separations and losses). This implies the development of subclinical signs and symptoms that signal the imminent failure occurring before the onset of the disease (differential diagnosis with adolescent adjustment disorder). This trend may have:
- Acute phase (in days or weeks) with a feeling of sudden break with the past and positive rapid onset of classic symptoms.
- Slow, insidious and subtle (in months or years) with progressive change in the way of being, usually in the earlier onset forms (which are the most disabling clinical course).
At this stage what occurs is:
- Emotional detachment with reduced expression of the emotions (affective coarctation) and flattening of affective relationships.
- Progressive difficulty in relation to isolation and social withdrawal (you leave school, friends, sports, hobbies and closed in a room or walking endlessly and aimlessly).
- Loss of interest motivation with the appearance of interests sometimes strange and magical themes of eccentric, pseudo-philosophical or pseudo-faced with an obvious lack of critical.
- Strange behavior / eccentric or impulsive, irritability (unprovoked aggression towards family, food, or inappropriate sexual behaviors).
- Impoverishment of the ideational content and the appearance of bizarre ways of thinking .
- Reduced social functioning and personal hygiene.
- Inability to perform peculiar tasks of their role.
- Progressive decline in attention, concentration, distractibility, impaired learning and performance at school and work.
- Anxiety that evolve in a vague sense of unease and fear in deep anguish.
- Perplexity
The Active Phase
In overt disease (active phase or period of state) there have been found positive symptoms, negative and disorganization variously associated.
Schizophrenia is characterized by two types of symptoms:
- Positive symptoms
- Negative Symptoms
Positive symptoms can be included under the term psychosis.
They are characterized by: obsessions, delusions, hallucinations and thought disorder.
Negative symptoms include a decline or disappearance of some of the skills of the person (emotional detachment, poverty of speech, decreased functions of communication, lack of motivation).
DIAGNOSIS
The diagnosis of schizophrenia requires the fulfillment of the following criteria:
A- (Symptoms and signs) The persistent presence of two or more of the following symptoms for a significant period of time that is considered at least a month (it appears that the duration may be less if the problem recedes following treatment):
- Delusions
- Hallucinations
- Disruption of verbal discourse (eg. losing the thread, incoherence, digression and expression are too abstract)
- Severe disorganization of behavior (eg. in clothing, diurnal habits, sleep disturbances, dysphoria, laugh or cry frequently and inappropriately), or been severely catatonic.
- Presence of negative symptoms, that convey a strong sense of disinterest, distance or absence of the subject: affective flattening (lack or strong reduction of emotional responses), alogia , avolizione (lack of motivation), attention deficit disorder and intellectual capacity, lack of eye contact.
B- Deficits or social dysfunction and / or employment: For a significant period of time one or more major areas of the subject's life are in serious jeopardy than before the onset of the disorder (work, interpersonal relationships, body care, nutrition, etc..)
C- Duration: persistence of symptoms "B" for at least six months, including at least a month of persistent symptoms of "A".
Note: The fulfillment of the criterion A is the only required (eg. the diagnosis is not required for the fulfillment of points B and C) only if the fixed ideas are bizarre and unrealistic, if hallucinations consist of hearing two or more unreal voices that speak to each other, or hearing a voice that "says" live the actions and perceptions of the patient.
DIAGNOSTIC PROCEDURES OF FUNCTIONAL NEUROIMAGINING
The Functional Neuroimaging is the use of neuroimaging technology to measure brain metabolism, in order to analyze and study the relationship between the activity of certain specific brain areas and brain functions.
The most commonly used methods include positron emission tomography (PET), functional magnetic resonance (fMRI), the multichannel EEG (EEG), the Single-photon emission computed tomography (SPECT), the magnetoencephalography (MEG) and the infrared spectroscopy (NIRS).
PET, fMRI, NIRS and SPECT measure changes in blood flow, related to the increase of cellular activity and thus neuronal activity. These changes in flow regions are defined as "active". The areas of the brain that are activated when the subject performs a particular task play a key role in the understanding of behavior, emotions, cognitive function and neural substrate.
The technique to observe the areas activated during a particular task requires multiple scans of brain activity. Activity is detected primarily "at rest", ie in the context of experimental research, but without the specific task. Next activity is detected during the task. The difference between the two maps can identify areas activated specifically during that particular task.
MEG and EEG record neural activity directly in the form of electromagnetic radiation, instead of PET images, SPECT and fMRI images that return indirect neuronal activity (for example, by studying in SPECT cerebral blood flow).
LABORATORY TEST
Lab tests may help to highlight the physical processes that underlie the patient's symptoms. The tests currently in use include various techniques for the representation of the brain, blood and urine tests, and analysis of the endocrine function of neurotransmitters and the use of EEG to evaluate the electrical activity of the brain.
NEUROCHEMICAL TESTS
Dexamethasone-suppression test
5-HIAA excreation test
ETIOLOGY and PATHOGENESIS
There is no single cause that leads to the occurrence of this disease. It would seem to be involved:
- Alterations in neurotransmission
- Morphologic modifications(investigated by diagnostic imaging and parallel with the theory of fractals)
- Risk factors
1. ALTERATIONS IN NEUROTRANSMISSION
The dopamine theory is among the hypotheses of the pathophysiological causes of schizophrenia.
Dopaminergic hypotheses
The symptoms of schizophrenia are due to hyperactivity of the dopaminergic system, especially in its mesolimbic component at post synaptic.
Dopaminergic system
The dopamine system is composed of three main ways:
The main neurotransmitter in this system is the dopamine, a noradrenaline precursor that works on five different subclasses of receptors:
- D1 e D5 : involved in the stimulation of the adenylate cyclase
- D2, D3 e D4 : involved in the inhibition of the adenylate cyclase

The receptors D1 and D2 (pre and post-sinaptic) are involved in the modulation of psychomotor systems , while in the schizophrenia the activation of these receptors causes hallucinations, delusions, paranoia (positive symptoms).
The receptors D3 and D4 are located most of all in areas mainly involved in the origin of the schizophrenia negative symptoms.

Evidence of this hypothesis is:
- L-DOPA worsen symptoms in schizophrenic patients; it may lead to onset of hallucinations in patients with Parkinson
- The DA receptor antagonists are effective in the treatment of schizophrenia.
- It is possible to observe increased levels of DA and HVA (homovanillic acid) in the striatum and cortex of schizophrenic patients (post-mortem)

- It is possible to observe an increase of DA D2 receptors in striatal and limbic brain of schizophrenics (post-mortem)
- PET Studies in vivo show, with some variability, an increase of D2 receptors in the brains of schizophrenics and an increase of DA release in response to apomorphine compared to controls.
However, other neurotransmitter systems seem to be involved In schizophrenia,:
- Serotonergic system :Serotonin inhibits the firing of dopaminergic neurons in striatal and mesolimbic level.

- Noradrenergic and gabaergic systems
- Cotrasmitter and neuro peptides: cholecystokinin, which is located in the dopaminergic neurons of the mesolimbic system and the Nerve growth factor which has recently been implicated as important cofactor in the mechanisms leading to this disease.
- Glutamatergic system : less neurotransmitter release in schizophrenic patients.
2. MORPHOLOGIC MODIFICATIONS

Through the observation of magnetic resonance imaging studies of schizophrenic patients, it has been possible to observe brain abnormalities.
These changes include:
- Expansion of the lateral ventricles (reported by 80% of studies)
- Expansion of the third ventricle (73% of studies)
- Involvement of the medial temporal lobe structures (74% of studies) such as the amygdala, hippocampus, parahippocampus around and neocortical temporal lobe regions.
If studies evaluating both the white matter and the gray matter are taken into consideration, in the temporal superior circle, abnormalities can be highlighted in 67% of the cases.
It Has also been reported evidence of abnormal frontal lobe (59% of studies), particularly the prefrontal gray matter and orbitofrontal regions in frontal and subcortical abnormalities.
These abnormalities seem to cause a disturbance in the connection between the various regions of the brain inside these regions. This is probably originated in the course of neurodevelopment.
Several theories have been proposed in the attempt to understand the implication of so many brain regions in schizophrenia, many of which are functionally related to each other.
Some researchers have hypothesized that abnormalities in the thalamus and its connections with the cortex and the cerebellum can cause a sort of cognitive dysmetria .
Others have focused their attention on the frontal lobes, basal ganglia and connections with the temporal lobe.
In contrast to the hypothesis that schizophrenia may be considered a neurodevelopmental encephalopathy, it has been proposed a model of disconnection in order to explain how changes in the temporal lobe may interrupt the connections between the limbic and prefrontal regions of the temporo-and vice versa.
A New Frontier: the Fractals
The fractal dimension (FD) was used to highlight the findings of brain structural irregularities in schizophrenic patients. This new approach seems to be a useful way to quantify the complexity of the bound form cerebral convolutions of the human brain.
But what is meant by fractal dimension?
A fractal is a geometric object that is repeated in its structure the same on different scales, this means that changes appearance even when viewed through a magnifying glass. There is a wide variety of objects that are defined but each manifests fractal variables. It 'so good to have these common characteristics of these objects.

Nature produces many examples of shapes very similar to fractals. For example, in a tree (especially in spruces) each branch is roughly similar to the entire tree and each branch in turn is similar to their own branch, and so on. It is also possible to see phenomena of self-similarity in the shape of a coast : with even larger satellite images, you can see that the general structure of more or less indented bays shows many components that, if not identical to the original, they look pretty much the same. According to Mandelbrot, the relationship between fractals and nature are deeper than you think.
« They believe that, in some way or the other, fractals have connections with the structure of the human mind. It is for this very reason that people find them so familiar. This familiarity still remains a mistery and the more they delve into this topic, the more the mistery increases. »
Benoit Mandelbrot
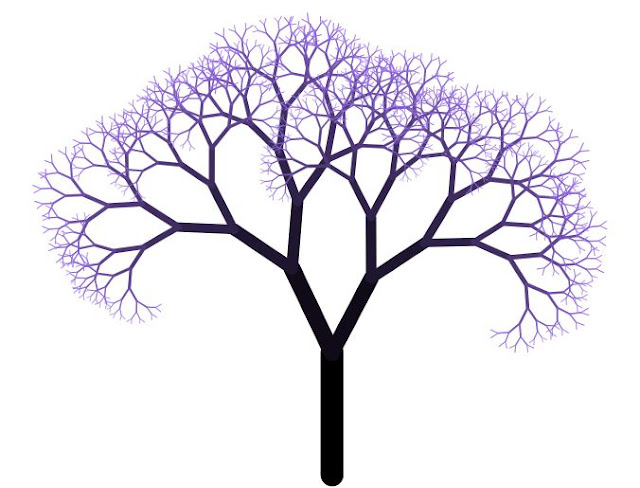
Fractals are used to find a new representation that starts from the basic idea that the small in nature is nothing but a copy of the great. Several mathematicians and physicians, observing and studying the physiology of the human body, found the structures and geometric forms of fractal figures and were able to apply everything that has been presented so far, to organs, tissues and cells.
A significant example of fractal theory applied to biology is the neuronal structure.
Neurons are cells used for the collection and transfer of information from all parts of our body in the form of electrical impulses. These signals are collected by means of thin cytoplasmic extensions, called dendrites, which then transfer them to the cell body. Information can be sent to adjacent neurons and move it throughout the body to reach the affected area. The fractal approach of these cells is clear by looking at the dendrites at high magnification level: on the larger ramifications there are other smaller.
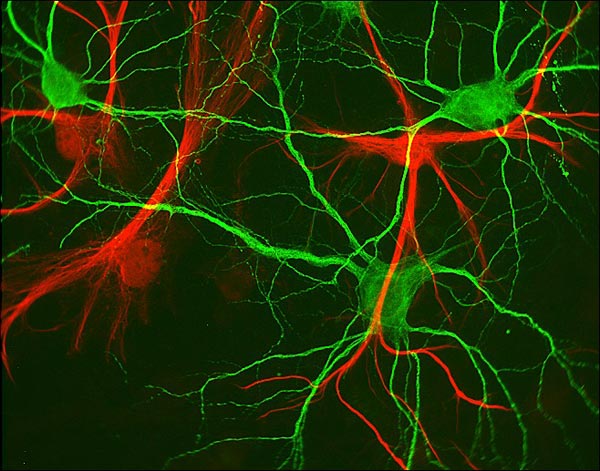
The fractal dimension can serve the classification of neurons based on morphological characteristics of the branches. Starting from some basic parameters, it is possible to start the analysis of fractal geometry applied to a given cell of the organism, a tissue or to a specific organ. With regard to nerve cells, their functions are largely dependent on its structure. To understand how a neuron integrates synaptic thousands of points, in order to generate an appropriate response, it requires the complete knowledge of geometry and cell morphology.
You can forward this brief classification:
- There are biological fractal structures beyond a certain point pass into a new shape and functions of different fractal (trachea and bronchial tree).
- There are fractal isolated biological structures, but which are linked to a higher-order fractal (many types of neurons of the cerebral convolutions with the macroscopic system. An example of these neurons are the Purkinje cells with their dendrites which are characteristic of fractal structures because the main branches are divided into small extensions to scalar relationships, consistent with each other.)
- Isolated biological structures fractals (bird feathers)
Through the observation of MR images from patients with schizophrenia compared to healthy controls, it was found the FD (fractal dimension), taking into account the following parameters according to some mathematical methods that take into consideration the ratio of gray matter / white matter, total cranial volume, relief morpho - structural each hemisphere.
The results have shown that schizophrenics have larger values of FD compared with healthy controls, in relation to the total cranial volume and in reference to the right hemisphere.
3. RISK FACTORS
Genetic Factors
Several genes are involved in the pathogenesis of schizophrenia, but nobody has an important role so as to be recognized as the only candidate gene.
Among the possible genes involved, studies have been conducted on:
Environment and Social Factors
There are several theories that are based on the concept of conflict and disharmony within the family as a contributory cause of schizophrenia.
THERAPY
Today you can get complete remissions by the critical phases and significant improvement of cognitive, affective and relational in the residual phases.
You can also start early treatment with a significantly lower risk of developing the disorder.
The main treatments for schizophrenia are called antipsychotics. Antipsychotics help
treating the positive symptoms of schizophrenia, helping to correct an imbalance in chemical reactions allow brain cells to communicate with each other.
As is the case for drug treatments for other illnesses, many patients with serious mental illness need to try several before finding an antipsychotic drug, or combination of medications, that works best for them.
- The Conventional Antipsychotics were introduced in the 50s and all had the same ability to treating the positive symptoms of schizophrenia. Most of these early antipsychotics "conventional" products differed in side effects.
These conventional antipsychotics include:
» chlorpromazine (Thorazine)
» fluphenazine (Anatensol, Moditen)
» haloperidol (Haldol)
» trifluoperazine (Modalina)
» perphenazine (Trilafon)
» thioridazine (Mellaril)
- The new "atypical" antipsychotics. Over the past ten years have introduced new "atypical" antipsychotics.
Compared to older antipsychotic "conventional", these drugs appear to be equally effective
in reducing positive symptoms such as hallucinations and delusions - but are they better in raising the negative symptoms of the disease, such as apathy, thinking problems, and lack of energy.
The atypical antipsychotics include:
» risperidone (Risperdal)
» clozapine (Clozaril)
» olanzapine (Zyprexa),
» quetiapine (Seroquel)
» ziprasidone (not yet commercially available in Italy)
- The current treatment guidelines recommend the use of an atypical antipsychotic, clozapine, in part, as a first treatment option for new patients. Instead, for patients who already benefit from treatment with conventional antipsychotics, atypical with a replacement may not be the best choice. Those wishing to change their medication should always consult your health care work together to develop the treatment plan more effective and safe as possible.
The therapy also includes a psycho-social rehabilitation.
Research shows that people with schizophrenia who attend structured programs, psychosocial rehabilitation, and continue with medication, better manage the disease and getting a better quality of life.
What are the side effects of medications used to treat schizophrenia?
All medicines have side effects.
Different medications produce different side effects, and people differ in both quantity and severity of side effects they experience.
Side effects can be treated by changing the dose of medication, changing the type of medication or treating the side effects directly, by other medications.
The most common side effects of antipsychotic drugs are: dry mouth, constipation, blurred vision, drowsiness.
Some people experience sexual dysfunction or decreased sexual desire, changes in
menstrual cycle and significant weight gain. Other common side effects are related and motor problems. These side effects include: agitation, rigidity, tremors, muscle spasms, and one of the most unpleasant and serious side effects, a condition called tardive dyskinesia.
Tardive dyskinesia is a movement disorder, which occurs in uncontrolled facial movements and sometimes shooting or twisting movements of other body parts. This condition usually develops after several years of treatment with antipsychotic drugs, and to a greater extent in older adults. Tardive dyskinesia affects 15 to 20% of those treated with conventional antipsychotics. The risk of being affected by tardive dyskinesia is lower for those taking the newer antipsychotics. Tardive dyskinesia can be treated with other drugs or reducing the dosage of the antipsychotic, if possible.
Serena Del Peschio
Annalisa