Bromazepam (marketed under several brand names, including Lectopam, Lexotan, Lexilium, Lexaurin, Brazepam, Rekotnil, Bromaze and Lexotanil) is a benzodiazepine derivative drug, patented by Roche in 1963 and developed clinically in the 1970s. It has mainly anxiolytic properties and at higher doses also sedative, hypnotic and skeletal muscle relaxant properties.

Systematic (IUPAC) name:9-bromo-6-pyridin-2-yl- 2,5-diazabicyclo [5.4.0]undeca- 5,8,10,12-tetraen- 3-one
INDICATIONS
For the short-term treatment of insomnia, short-term treatment of anxiety or panic attacks, if a benzodiazepine is required, and the alleviation of the symptoms of alcohol- and opiate-withdrawal. Premedication to alleviate anxiety before surgery.
Biotransformation
Hepatically, via oxidative pathways (via an enzyme belonging to the Cytochrome P450 family of enzymes).
Absorption
Bioavailability is 84% following oral administration.
Half-Life
10-20 hours.
SIDE EFFECTS
Bromazepam 3 times 6 mg daily for 2 weeks taken alone impaired learning capacities significantly in humans in an experiment. In combination with alcohol the impairments of learning capacity became even more pronounced. Impairments to memory functions are common with bromazepam and include a reduced working memory and reduced ability to process environmental information. Impaired memory, visual information processing and sensory data and impaired psychomotor performance.
Deterioration of cognition including attention capacity and impaired co-ordinative skills. Impaired reactive and attention performance, which can impair driving skills.
The most common side-effects of benzodiazepines are related to his sedating and muscle-relaxing action. They include drowsiness, dizziness, and decreased alertness and concentration. Lack of coordination may result in falls and injuries, in particular, in the elderly. Another result is impairment of driving skills and increased likelihood of road traffic accidents. Decreased libido and erection problems are a common side effect. Depression and disinhibition may emerge. Hypotension and suppressed breathing may be encountered with intravenous use.
Paradoxical effects
Paradoxical reactions, such as increased seizures in epileptics, aggression, violence, impulsivity, irritability and suicidal behavior sometimes occur. These reactions have been explained as consequences of disinhibition and the subsequent loss of control over socially unacceptable behavior. Paradoxical reactions are rare in the general population, with an incidence rate below 1% and similar to placebo. However, they occur with greater frequency in recreational abusers, individuals with borderline personality disorder, children, and patients on high-dosage regimes. In these groups, impulse control problems are perhaps the most important risk factor for disinhibition; learning disabilities and neurological disorders are also significant risks. Most reports of disinhibition involve high doses of high-potency benzodiazepines. Paradoxical effects may also appear after chronic use of bromazepam.
Cognitive effects
The short-term use of benzodiazepines adversely affects multiple areas of cognition, the most notable one being that it interferes with the formation and consolidation of memories of new material and may induce complete anterograde amnesia. However, researchers hold contrary opinions regarding the effects of long-term administration. One view is that many of the short-term effects continue into the long-term and may even worsen, and are not resolved after quitting benzodiazepines. Another view maintains that cognitive deficits in chronic benzodiazepine users occur only for a short period after the dose, or that the anxiety disorder is the cause of these deficits.
Long-term effects
Adverse effects of chronicbromazepam use can include cognitive impairment as well as affective and behavioural problems. Feelings of turmoil, difficulty in thinking constructively, loss of sex-drive, agoraphobia and social phobia, increasing anxiety and depression, loss of interest in leisure pursuits and interests, and an inability to experience or express feelings can also occur. Additionally an altered perception of self, environment and relationships may occur.
Other effects
Very rarely dystonia can develop.
Leukopenia and liver-damage of the cholostatic type with or without jaundice (icterus) have additionally been seen.
Up to 30% treated on a long-term basis develop a form of dependence, i.e. these patients cannot stop the medication without experiencing physical and/or psychological benzodiazepine withdrawal symptoms.
Ambulatory patients should be warned that Bromazepam may impair the ability to drive vehicles and to operate machinery. The impairment is worsened by consumption of alcohol, because both act as central nervous system depressants. During the course of therapy, tolerance to the sedative effect usually develops.
Less common side effects include nausea and changes in appetite, blurred vision, confusion, euphoria, depersonalization and nightmares. Cases of liver toxicity have been described but are very rare.
Chemical gastritis after chronic bromazepam intake: a case report.
Background:
a rare case of diffuse macroscopic discoloration and chemical gastritis due to chronic bromazepam intake. The chemical composition of pharmaceuticals has to be considered at endoscopy and it is evident that some chemical substances damage the epithelial tissue and lead to clinical symptoms.
 Endoscopy appearance of the gastric antrum with discoloration after bromazepam intake.
Endoscopy appearance of the gastric antrum with discoloration after bromazepam intake.
Case Presentation
Endoscopy was performed in an 82-year-old patient due to gastroesophageal reflux symptoms and epigastric pain. Gastroscopy showed a hiatal hernia and a scarred duodenal bulb. More striking was the yellow-brownish discoloration of the gastric and the duodenal mucosa. The gastric antrum and the duodenal bulb showed local discoloration that could not be rinsed off. The medical history indicated that bromazepam (6 mg) had been used daily as a sleeping aid in the previous two years. The histopathological findings showed appearances of chemical gastritis. Within the lamina propria and on the epithelial surface there were granules. There was no foreign body reaction to these granules. Corpus mucosa showed a mild chronic gastritis.
 Discoloration of the duodenal bulb after bromazepam intake.
Discoloration of the duodenal bulb after bromazepam intake.
Conclusions
If discoloration of the mucosa at endoscopy is seen, a careful drug history must be sought. This is the first case in literature that shows a chemical gastritis after bromazepam intake.
TOLERANCE, DEPENDENCE AND WITHDRAWAL
Bromazepam shares with other benzodiazepines the risk of abuse, misuse, psychological dependence and/or physical dependence. A withdrawal study demonstrated both psychological dependence and physical dependence on bromazepam including marked rebound anxiety after 4 weeks chronic use. Those whose dose was gradually reduced experienced no withdrawal.
Patients treated with bromazepam for generalised anxiety disorder were found to experience withdrawal symptoms such as a worsening of anxiety, as well as the development of physical withdrawal symptoms when abruptly withdrawn from bromazepam. Abrupt or over rapid withdrawal from bromazepam after chronic use even at therapeutic prescribed doses can lead to a severe withdrawal syndrome including status epilepticus and a condition resembling delirium tremens.
Animal studies have shown that chronic administration of diazepam or bromazepam causes a decrease in spontaneous locomotor activity and the turnover of noradrenaline and dopamine and serotonin, decreased activity of tyrosine hydroxylase and increased levels of the catecholamines. During withdrawal of bromazepam or diazepam a fall in tryptophan, 5-hydroxytryptamine levels occurs as part of the benzodiazepine withdrawal syndrome.

Contraindications and special precautions
Benzodiazepines require special precaution if used in the elderly, pregnancy, children, alcohol- or drug-dependent individuals and individuals with comorbid psychiatric disorders.
Special Populations
Elderly
In 1987, a team of scientists led by Ochs reported that the elimination half-life, peak serum concentration, and serum free fraction are significantly elevated and the oral clearance and volume of distribution significantly lowered in elderly subjects. The clinical consequence is that the elderly should be treated with lower doses than younger patients.
Driving
Bromazepam may affect driving and ability to operate machinery.
Pregnancy and breast feeding
Bromazepam is pregnancy category D, a classification which means that bromazepam has been shown to cause harm to the unborn child. There has been at least one report of sudden infant death syndrome linked to breast feeding, while consuming bromazepam.
PHARMACOLOGY
Bromazepam is a "classical" benzodiazepine; other classical benzodiazepines include diazepam, clonazepam, oxazepam, lorazepam, nitrazepam, flurazepam and clorazepate. Its molecular structure is composed of a diazepine connected to a benzene ring and a pyridine ring, the benzene ring having a bromine atom attached to it. It is a 1,4-benzodiazepine, which means that the nitrogens on the seven-sided diazepine ring are in the 1 and 4 positions.
Bromazepam binds to the GABA receptor GABAA , causing a conformational change and increasing inhibitory effects of GABA .
Other neurotransmitters are not influenced. Bromazepam is intermediate-short acting benzodiazepine and is lipophilic.
After night time administration of bromazepam a highly significant reduction of gastric acid secretion occurs during sleep followed by a highly significant rebound in gastric acid production the following day.
Bromazepam alters electrical status of the brain causing an increased beta activity and a decrease in alpha activity in the EEG recordings.

MECHANISM OF ACTION
Benzodiazepines work by increasing the efficiency of a natural brain chemical, GABA, to decrease the excitability of neurons. This reduces the communication between neurons and, therefore, has a calming effect on many of the functions of the brain.
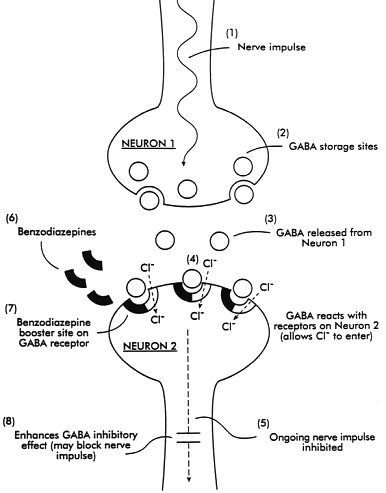
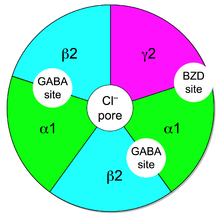
GABA controls the excitability of neurons by binding to the GABAA receptor. The GABAA receptor is a protein complex located in the synapses of neurons. All GABAA receptors contain an ion channel that conducts chloride ions across neuronal cell membranes and two binding sites for the neurotransmitter gamma-aminobutyric acid (GABA), while a subset of GABAA receptor complexes also contain a single binding site for benzodiazepines. Binding of benzodiazepines to this receptor complex promotes binding of GABA, which in turn increases the conduction of chloride ions across the neuronal cell membrane. This increased chloride ion conductance hyperpolarizes the neuron's membrane potential. As a result, the difference between resting potential and threshold potential is increased and firing is less likely.
The subset of GABAA receptors that also bind benzodiazepines are referred to as benzodiazepine receptors (BzR). The GABAA receptor is a heteromer composed of five subunits, the most common ones being two αs, two βs, and one γ (α2β2γ). GABAA receptors that are made up of different combinations of subunit subtypes have different properties, different distributions in the brain and different activities relative to pharmacological and clinical effects. Benzodiazepines bind at the interface of the α and γ subunits on the GABAA receptor. Binding also requires that alpha subunits contain a histidine amino acid residue, (i.e., α1, α2, α3, and α5 containing GABAA receptors). For this reason, benzodiazepines show no affinity for GABAA receptors containing α4 and α6 subunits with an arginine instead of a histidine residue.
Once bound to the benzodiazepine receptor, the benzodiazepine ligand locks the benzodiazepine receptor into a conformation in which it has a greater affinity for the GABA neurotransmitter. This increases the frequency of the opening of the associated chloride ion channel and hyperpolarizes the membrane of the associated neuron. The inhibitory effect of the available GABA is potentiated, leading to sedatory and anxiolytic effects.
Bromazepam and benzodiazepines also interact with peripheral benzodiazepine receptors. Peripheral benzodiazepine receptors are present in peripheral nervous system tissues, glial cells, and to a lesser extent the central nervous system. These peripheral receptors are not structurally related nor coupled to GABAA receptors. They modulate the immune system and are involved in the body response to injury. Benzodiazepines also function as weak adenosine reuptake inhibitors. It has been suggested that some of their anticonvulsant, anxiolytic and muscle relaxant effects may be in part mediated by this action.
PHARMACOKINETICS
Benzodiazepines relatively rapidly cross the blood-brain barrier and equilibrate with brain tissue. The two principal pathways of the BDZ biotransformation involve hepatic microsomal oxidation, N -dealkylation or aliphatic hydroxylation and glucuronide conjugation. The metabolites are excreted mainly by the kidney.
Bromazepam is reported to be metabolized by a hepatic enzyme belonging to the Cytochrome P450 family of enzymes. In 2003, a team led by Dr. Oda Manami at Oita Medical University reported that CYP3A4 was not the responsible enzyme, seeing as itraconazole, a known inhibitor of CYP3A4, did not affect its metabolism. In 1995, J. van Harten at Solvay Duphar B.V.'s Department of Clinical Pharmacology in Weesp reported that fluvoxamine, which is a potent inhibitor of CYP1A2, a less potent CYP3A4 inhibitor, and a negligible inhibitor of CYP2D6, does inhibit its metabolism.

Overdose
Although benzodiazepines are much safer in overdose than their predecessors, the barbiturates, they can still cause problems in overdose.Taken alone, they rarely cause severe complications in overdose; statistics in England showed that benzodiazepines were responsible for 3.8% of all deaths by poisoning from a single drug. However, combining these drugs with alcohol, opiates or tricyclic antidepressants markedly raises the toxicity. The elderly are more sensitive to the side effects of benzodiazepines, and poisoning may even occur from their long-term use.
The symptoms of a benzodiazepine overdose may include; drowsiness, slurred speech, nystagmus, hypotension, ataxia, coma, respiratory depression, and cardiorespiratory arrest.
Bromazepam is commonly involved in drug overdoses.Bromazepam is a drug sometimes used in suicide attempts. A severe bromazepam benzodiazepine overdose may result in an alpha pattern coma type. The toxicity of bromazepam in overdosage increases when combined with other CNS depressant drugs such as alcohol or sedative hypnotic drugs.Bromazepam is the most common benzodiazepine involved in intentional overdoses in France.
References